Cumberland Public Health Annual Report 2025
Cumberland Public Health Annual Report 2025 alynchOur increasingly ageing population is one of the great triumphs of society. Better living conditions and significant improvements in medical care mean that more people are living longer lives than at any point in history – surely something to be celebrated. But it brings with it some substantial challenges. The number of older people leaving the workforce and needing care is rising, and the capacity and resource to provide that care is increasingly stretched. When we hear headlines about the NHS being in crisis, this is one of the underlying challenges. It also underpins a narrative about there being a “pensions time bomb”, with a rising bill for pensions coupled with a reducing tax take from the younger population leading eventually to a position where our social security system becomes unaffordable. These challenges are very real.
But that does not mean an inexorable slide into social decline. We need a radical rethink on our approach to age and ageing. For too long, older people have tended to be seen in policy terms as a problem, or a burden on society. But the same things that have led to longer lives have helped extend healthy life, meaning that people can continue to be part of the solution for longer. Older people bring a wealth of skills, knowledge and experience that can add real value to the economy and to efforts to improve society. We need to shape a society that values older people, and helps them to remain nett contributors to society for as long as they can, before gratefully supporting them to live their final years with as much comfort and dignity as possible.
This report therefore concentrates on how we can promote healthier ageing in Cumberland. It starts by describing the current picture of our demography and the health challenges associated with ageing, before going on to describe our approach to helping Cumberland to become an age-friendly society. It then considers a number of crucial components of that society – social inclusion, housing, digital inclusion, and health and care support – in more detail. Finally, it considers the subject of Dying Well, something I first discussed in the Cumbria Public Health Annual Report in 2017. Since then, the movement supporting a more nuanced approach to death and dying has grown, but the statistics on the proportion of people dying in hospital have barely shifted, and hospices are finding themselves in increasingly challenging financial situations. I remain concerned that this universal human experience does not receive the attention that it deserves.
Society faces considerable challenges associated with an ageing population. However, if we can rethink our approach, become a truly age friendly society and focus services on preventing or significantly delaying some of the effects of ageing, we can create a society that can become “stronger with age”.
Colin Cox
Director of Public Health and Communities
United Kingdom
Introduction and Scope
Introduction and ScopeCumberland’s population is getting older, which brings both challenges and opportunities for health and social care. As people live longer, their healthcare needs become more complex, especially when it comes to end-of-life care. This annual report seeks to address these challenges by providing a comprehensive analysis of the current state of services for elderly residents, identifying gaps, and proposing evidence-based solutions to support healthier ageing and dignified end-of-life experiences.
The report aligns with Cumberland’s commitment to delivering compassionate, high-quality, and equitable care for all its residents, with a focus on older adults. It emphasises collaboration among health services, social care providers, community organisations, and policymakers to create a coordinated, person-centred approach to care. This document builds on national frameworks and local strategies, including the North Cumbria Partnership Board’s overarching frailty program and the principles outlined in the Ambitions for Palliative and End-of-Life Care framework. In the following sections, we explore the specific challenges and opportunities facing Cumberland’s ageing population, along with evidence-based recommendations for a more inclusive and supportive system.
Specifically, the report aims to:
Analyse the Demographic Landscape with an in-depth overview of Cumberland’s elderly population, including key health trends, social determinants of health, and service utilisation patterns.
Identify Critical Challenges: Highlight the major health and social care challenges faced by elderly residents, such as frailty, chronic conditions, and barriers to accessing care in rural areas.
Explore Collaborative Opportunities: Examine how community resources, primary care, and social services can better integrate to support elderly individuals.
Focus on End-of-Life Care: Assess the current state of palliative and end-of-life care services, drawing on insights from local hospice leaders and other stakeholders to improve quality and accessibility.
Make Evidence-Based Recommendations: Propose actionable strategies to enhance care delivery and outcomes for elderly residents.
The scope of this report aims to look at the full spectrum of elderly care, from promoting healthy ageing to managing complex health needs and ensuring dignity in death. By addressing these key areas, this report aims to provide a roadmap for improving the quality of life for elderly residents and ensuring that Cumberland remains a place where people can live, age and die well.
Chapter 1: The Ageing Population of Cumberland - Demographics and Health Insights
Chapter 1: The Ageing Population of Cumberland - Demographics and Health InsightsThe elderly population in Cumberland represents a significant and growing proportion of the community, bringing unique challenges and opportunities for health and social care services. Understanding the demographic characteristics and social determinants affecting older adults is essential for designing effective interventions and policies.
Current Demographic Data
Population Size
Cumberland’s population aged 65 and over has seen consistent growth in recent years, reflecting national trends of an ageing population. The 2021 Census data highlights that Cumberland has a significantly older population compared to both the Northwest region and England as a whole. As shown in Table 1, 23.2% of Cumberland’s population is aged 65 and over, exceeding the Northwest (18.7%) and England (18.4%) averages. This demographic trend indicates a clear shift towards an ageing population, with an increasing proportion of older residents compared to regional and national figures (ONS, 2023).
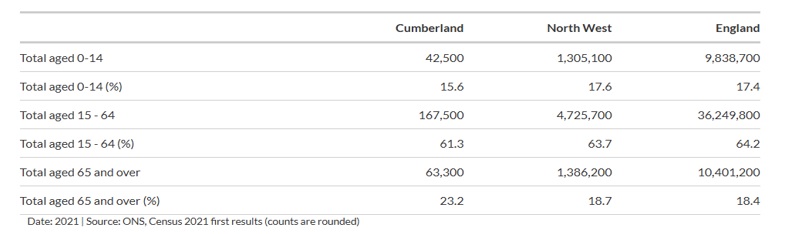
Table 1: Age Distribution in Cumberland, Northwest, and England
Source: ONS, Census 2021
Further demonstrating this trend, Figure 1 presents the population distribution by five-year age groups, comparing Cumberland with England. The graph shows that Cumberland has a noticeably larger proportion of older adults, particularly in the 65+ and 85+ age brackets, than the national average. The proportion of people aged 85 and over is projected to grow by over 30% in the next decade, highlighting a continuing demographic shift (Age UK, 2022).
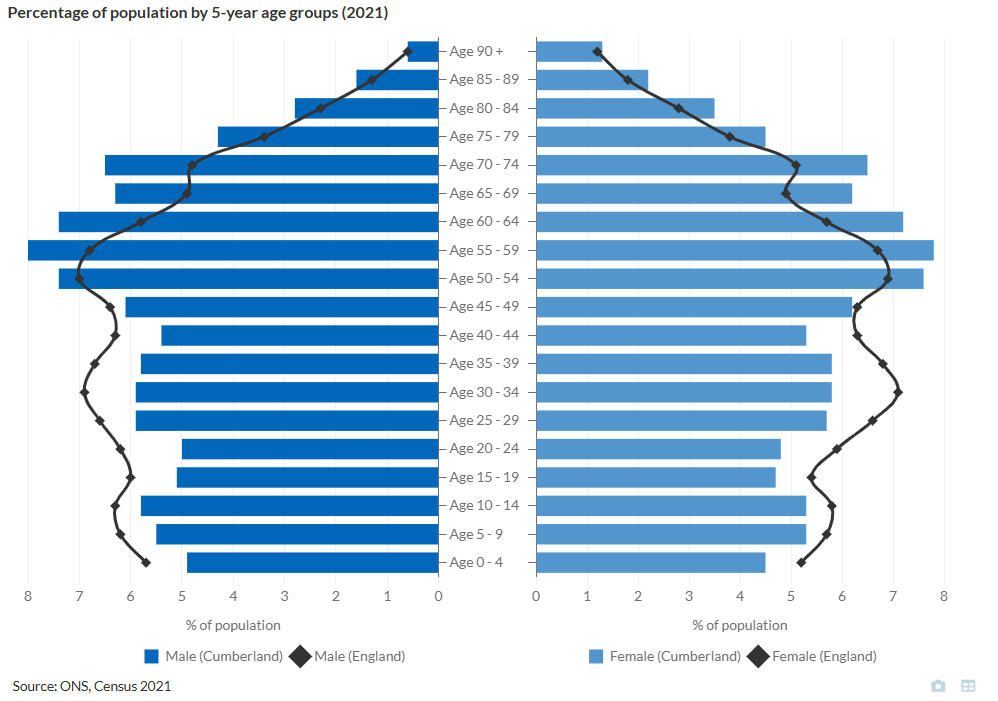
Figure 1: Population Distribution by 5-Year Age Groups in Cumberland and England
Source: ONS, Census 2021.
Geographical Distribution
Using the 2021 census data, we can breakdown Cumberland into districts and can see variation in the age distribution of people 65 and over in Cumberland.
| Area | Population 65+ (%) |
|---|---|
| Allerdale | 25 |
| Carlisle | 20 |
| Copeland | 21 |
Table 2: Population Aged 65 and Over by Area in Cumberland (2021 Census)
Source: ONS, Census 2021
Allerdale and Copeland are more rural than Carlisle, which has large rural areas but also a key urban centre that contains around half of its population. The higher percentage of older adults in Allerdale (25%) reflects a common trend observed in rural areas, where populations tend to age more rapidly. This is often due to younger people migrating towards urban centres like Carlisle in search of employment, education, and better access to services, leaving behind an older demographic in more remote locations.
Rurality presents unique public health challenges for these areas. Older adults in rural communities often face difficulties accessing primary care, specialist services, and emergency healthcare due to longer travel distances and fewer local facilities. Additionally, the lack of transport links and limited opportunities for social engagement can increase the risk of social isolation and loneliness, further impacting mental health and well-being.
Life Expectancy
Life expectancy in Cumberland is 79 years for men and 83 years for women, slightly below the national averages of 80 years for men and 84 years for women (Public Health England, 2023). However, these figures mask significant disparities in both total life expectancy and healthy life expectancy, particularly between rural and socioeconomically deprived areas.
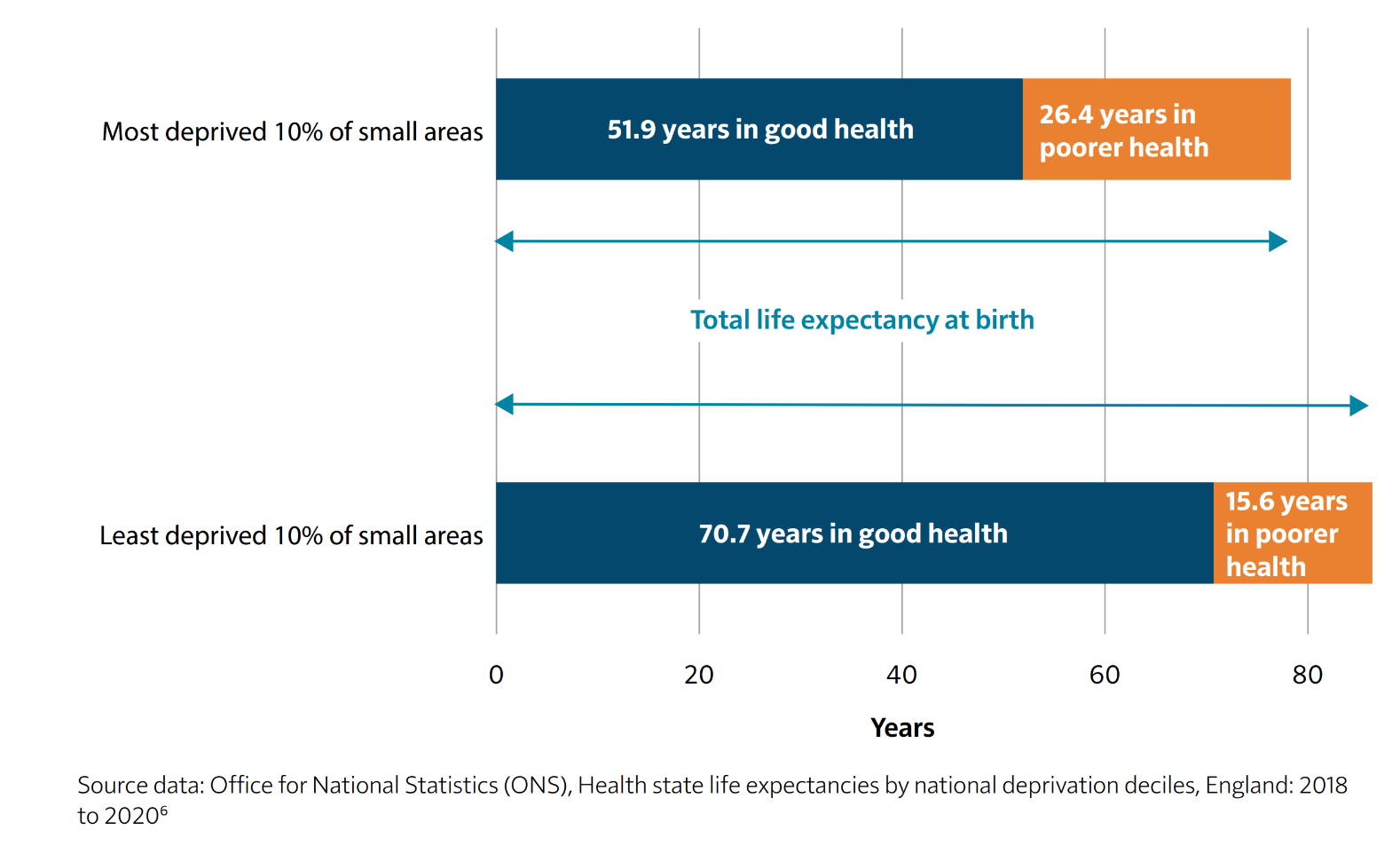
Figure 2: Life Expectancy and Healthy Life Expectancy by Deprivation Level in England (2018–2020)
Source: Office for National Statistics (ONS), Health State Life Expectancies by National Deprivation Deciles, England: 2018 to 2020.
As illustrated in Figure 2, individuals in the most deprived areas not only have shorter life expectancies but also spend a significantly larger proportion of their later years in poor health. In Cumberland’s more deprived communities, older adults face higher rates of long-term illness, poorer access to healthcare, and greater levels of social isolation, all of which contribute to a shorter life expectancy and lower quality of life in later years. The graph highlights that those in the most deprived areas spend an average of 26.4 years in poor health, compared to just 15.6 years in the least deprived areas, reflecting stark inequalities in healthy ageing.
Conversely, older adults in more affluent or rural parts of Cumberland tend to live longer and in better health, often benefiting from lower pollution levels, stronger social networks, and healthier lifestyles. However, even in these areas, challenges remain, particularly concerning access to healthcare services, availability of social care, and transportation barriers, all of which are crucial for supporting independent living among the elderly.
Healthy Life expectancy
Healthy life expectancy (HLE) is a crucial indicator of population health, representing the number of years an individual can expect to live in good health. It reflects not just longevity but also the quality of life and the effectiveness of local health and social care systems. In Cumberland, HLE trends suggest key challenges and disparities when compared to neighbouring areas such as Westmorland & Furness, wider Cumbria, and national averages.
Trends in Healthy Life Expectancy
Between 2012 and 2022, Cumberland has experienced a decline in HLE for both males and females. In 2012, male HLE at birth in Cumberland stood at 61.4 years, peaking at 62.81 years in 2016, before steadily declining to 58.38 years by 2022. Similarly, female HLE at birth started at 62.1 years in 2012, peaked at 63.96 years in 2016, and dropped to 59.13 years in 2022. This decline suggests increasing health inequalities and potential concerns regarding the effectiveness of preventive health measures and social care provision.
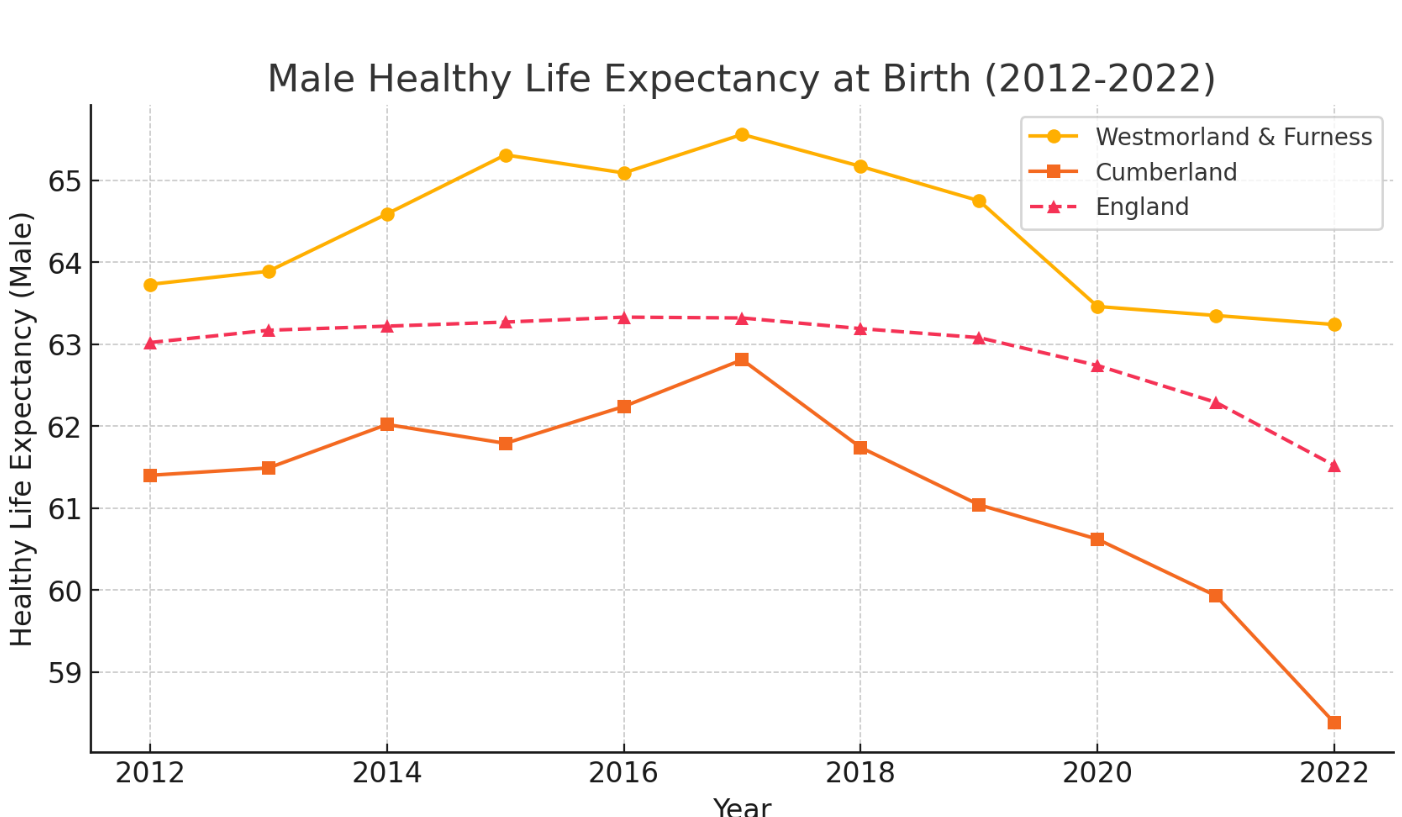
Figure 3: Male Healthy Life Expectancy at Birth in Cumberland, Westmorland & Furness, and England (2012–2022)
Source: Office for National Statistics (ONS), 2023.
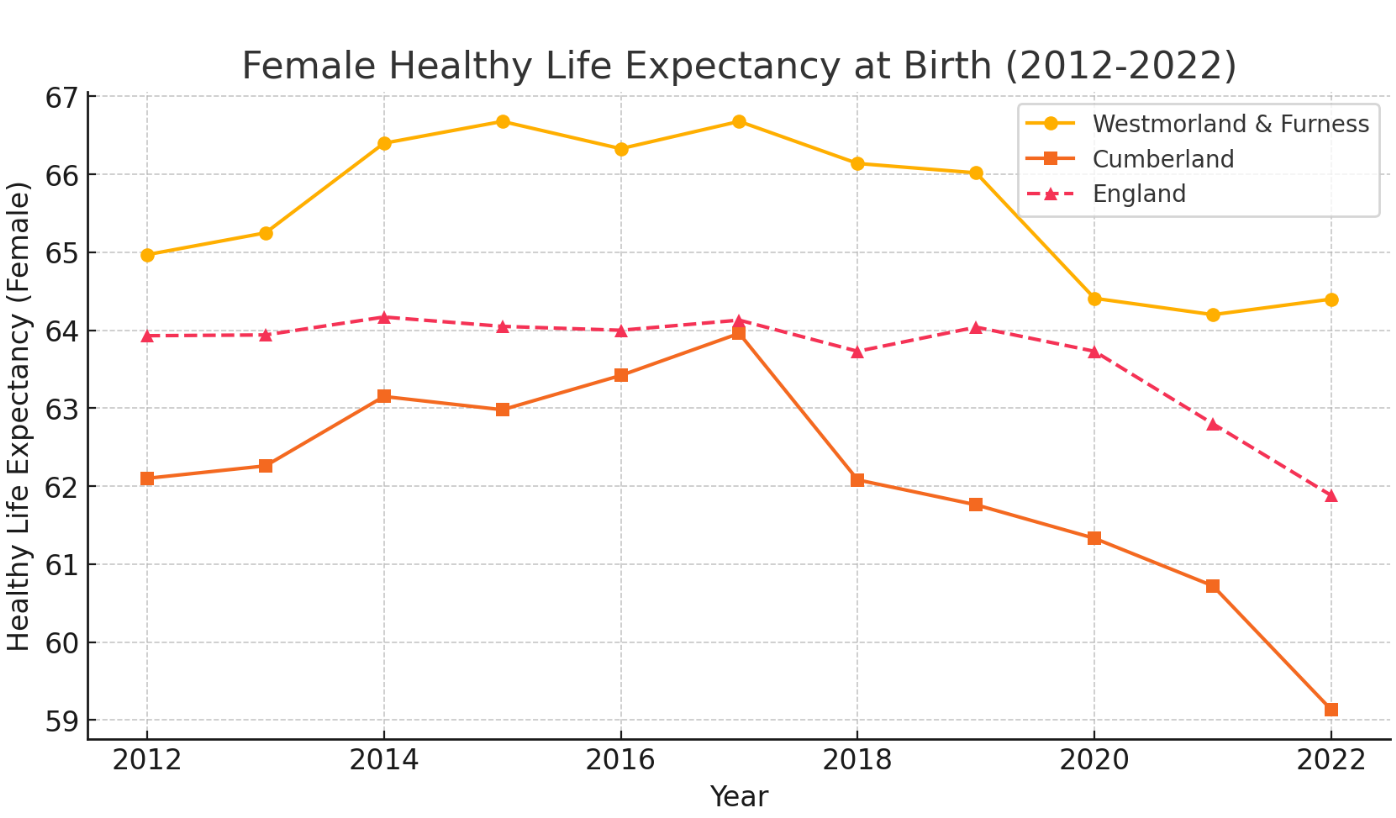
Figure 4: Female Healthy Life Expectancy at Birth in Cumberland, Westmorland & Furness, and England (2012–2022)
Source: Office for National Statistics (ONS), 2023.
In contrast, Westmorland & Furness has consistently demonstrated a higher HLE across the decade, because people in this area, on average, have higher incomes and better living conditions. Male HLE in 2012 was 63.73 years, rising to 65.56 years in 2017, before experiencing a slight decline to 63.24 years in 2022. Female HLE followed a similar trajectory, peaking at 66.68 years in 2014 and 2017, before decreasing to 64.4 years in 2022.
The higher HLE in Westmorland & Furness is strongly linked to socioeconomic advantages, as the region remains on average more affluent than Cumberland despite having some significant pockets of deprivation.
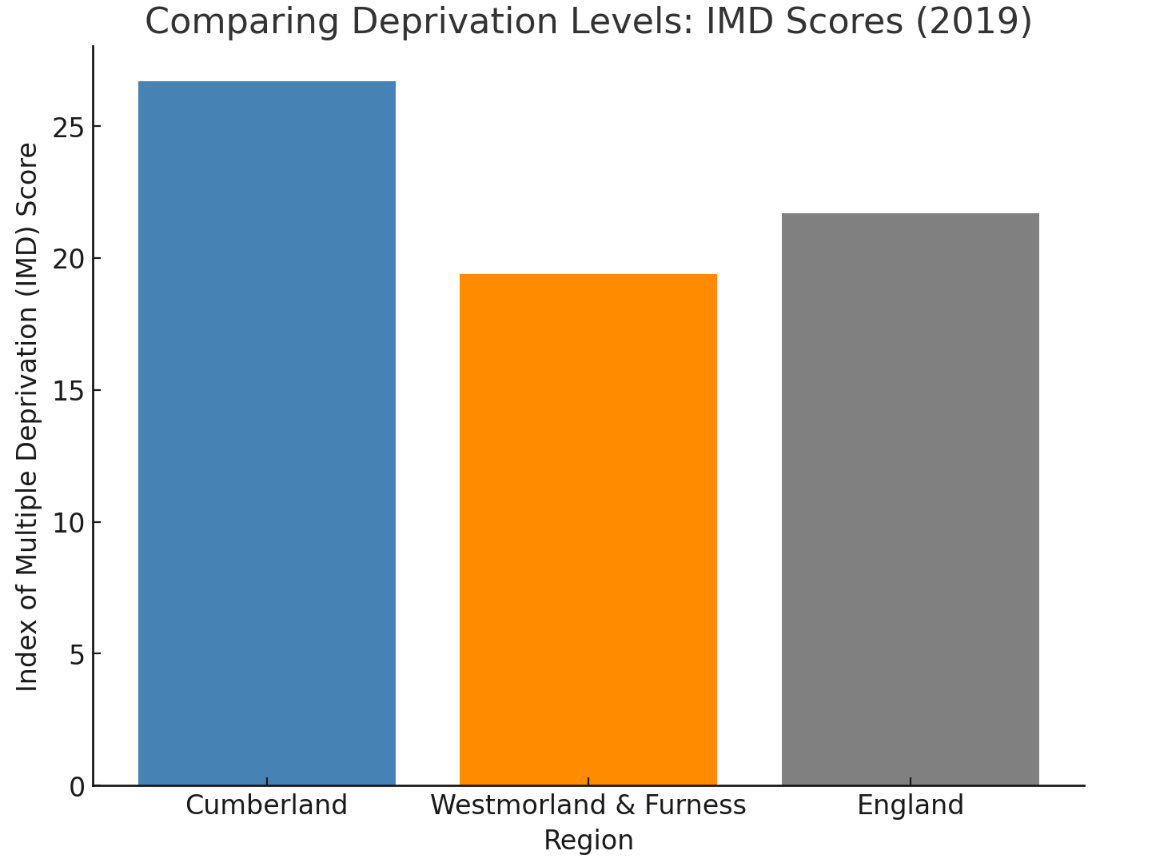
Figure 5: Comparing Deprivation Levels – Index of Multiple Deprivation (IMD) Scores (2019)
Source: English Indices of Deprivation, Ministry of Housing, Communities & Local Government (2019).
Higher income levels, better housing conditions, and increased access to preventive healthcare services contribute to healthier ageing outcomes (ONS, 2023; Public Health England, 2023). Socioeconomic disparities impact lifestyle choices, including diet, physical activity, and smoking prevalence, all of which are major determinants of HLE (The King’s Fund, 2023). In contrast, Cumberland has a higher proportion of deprived communities, which correlates with greater levels of long-term illness and earlier onset of frailty (Joseph Rowntree Foundation, 2023).
At the national level, England’s male HLE was 63.02 years in 2012, showing a gradual decline to 61.52 years by 2022, a trend mirrored in female HLE. This indicates a broader national issue of declining healthy years lived, potentially linked to factors such as an ageing population, increasing levels of chronic diseases, and the long-term impacts of economic and health inequalities.
Regional Disparities and Key Considerations
Comparing Cumberland’s figures to the wider Cumbria region, a similar pattern emerges, with the county's HLE being higher in more affluent and rural areas like Westmorland & Furness but declining in areas with higher levels of deprivation, including parts of Cumberland. This highlights persistent health inequalities within Cumbria, where variations in access to healthcare, employment opportunities, and social support networks play a significant role in determining health outcomes.
Excess Winter Deaths in Cumberland
Winter brings with it an increased risk of illness and mortality, particularly for older adults. Cold temperatures, seasonal infections, and fuel poverty contribute to excess winter deaths (EWD), which refer to the additional deaths occurring in the winter months compared to the rest of the year. Data from the Office for National Statistics (ONS) for 2020/21, which includes COVID-19-related deaths, reveals stark regional disparities.
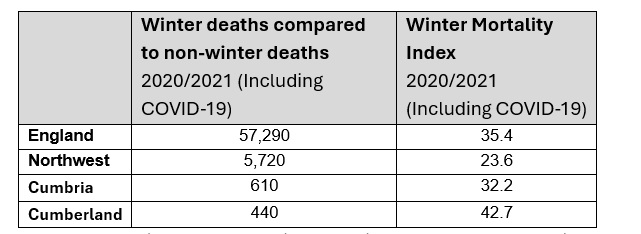
Table 3: Excess Winter Deaths and Winter Mortality Index (2020/2021, Including COVID-19)
Source: Office for National Statistics (ONS), 2021
Cumberland recorded 440 excess winter deaths, with a Winter Mortality Index (WMI) of 42.7 - the highest among the areas analysed. The WMI measures the percentage increase in deaths during the winter months (December to March) compared to the non-winter months, offering an indication of how significantly winter impacts mortality. A higher WMI suggests a greater seasonal effect on deaths. Cumberland’s WMI of 42.7 highlights that winter mortality in the area was disproportionately high compared to both the Northwest (23.6 WMI) and the national average (35.4 WMI). Cumbria as a whole also reported a higher-than-average WMI of 32.2, reinforcing the particular challenges faced by rural communities.
Several factors contribute to these figures. Older people are particularly vulnerable, with pre-existing conditions such as cardiovascular disease, respiratory illnesses, and frailty exacerbating the effects of cold weather. Housing conditions play a crucial role, as many older residents in Cumberland live in poorly insulated homes that are expensive to heat, increasing the likelihood of cold-related illnesses. The region’s rural geography also presents a challenge, with limited access to healthcare services making it harder to receive timely treatment during winter months.
The impact of COVID-19 cannot be overlooked. The pandemic placed additional strain on health services, while restrictions on social contact may have reduced the ability of families and carers to support elderly relatives, leading to delayed medical attention for winter-related illnesses.
Reducing Winter Mortality in Cumberland
A comprehensive approach is needed to tackle excess winter deaths in Cumberland, focusing on housing conditions and healthcare access. Cold homes significantly increase the risk of respiratory and cardiovascular illnesses, particularly in rural areas where older housing and off-grid energy make heating costly. To address this, affordable warmth initiatives should prioritise home insulation schemes, financial support for heating costs, and cold weather action plans providing fuel vouchers and emergency heating assistance.
Alongside housing improvements, better healthcare outreach is vital to prevent winter illnesses. Influenza and pneumonia remain leading causes of seasonal deaths, particularly for older adults with chronic conditions. However, vaccine uptake is lower in rural areas due to transport barriers and limited access to healthcare. Expanding mobile vaccination clinics, home visits, and targeted promotion through GP practices and pharmacies would help protect those most at risk. Strengthening partnerships between primary care, local councils, and community organisations can further improve vaccine access and winter health support. By tackling fuel poverty and healthcare access, Cumberland can reduce preventable winter deaths and improve outcomes for its ageing population.
Winter deaths are largely preventable, and targeted interventions could help reduce the seasonal strain on health and social care services. Ensuring that older adults in Cumberland remain warm, well-supported, and connected to healthcare in colder months is a public health priority.
The Burden of Disease and Chronic Conditions
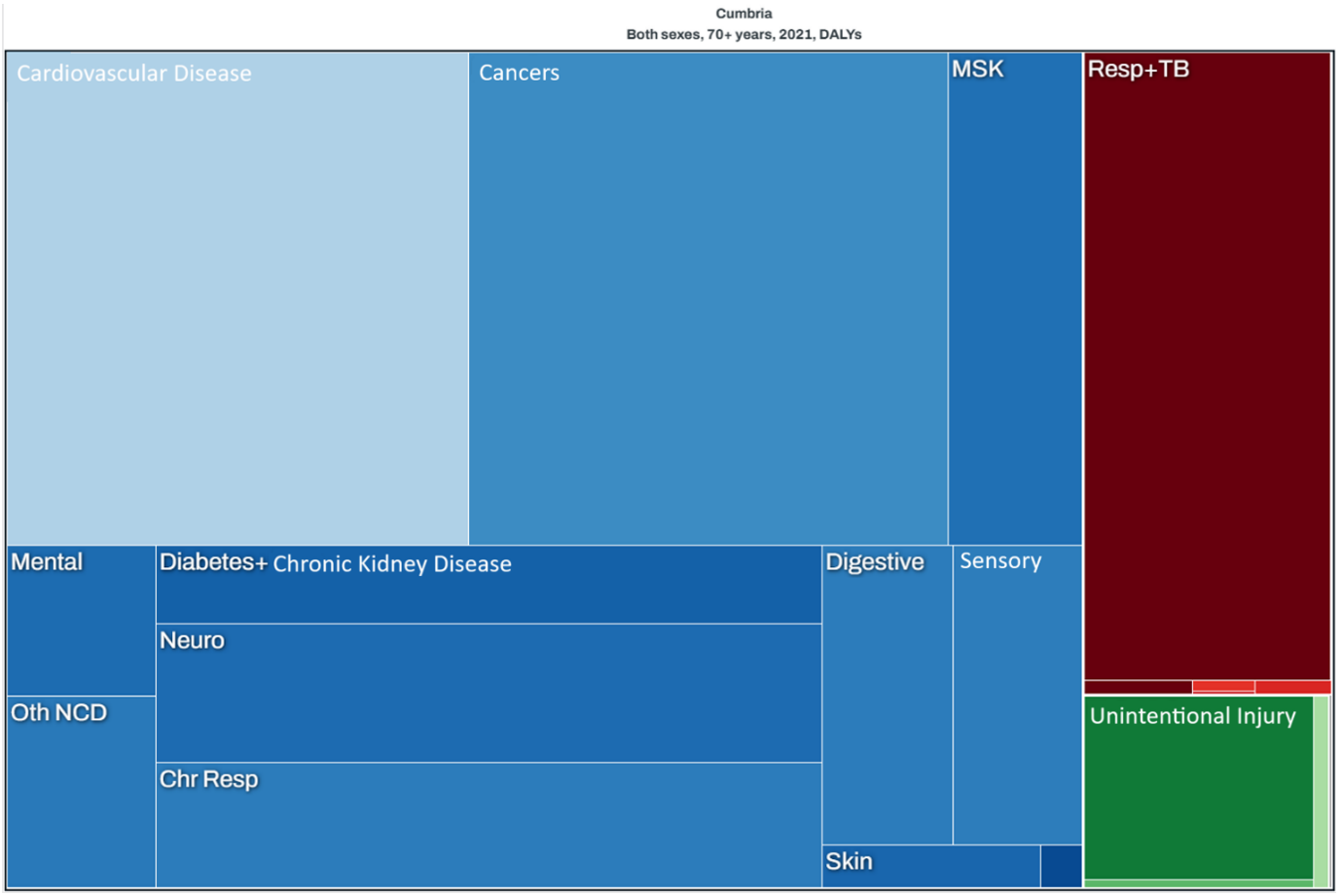
Figure 6: Burden of Disease in Cumbria (Both Sexes, 70+ Years, 2021) – Disability-Adjusted Life Years (DALYs)
Source: Global Burden of Disease Study, Institute for Health Metrics and Evaluation (IHME), 2021
The tree map, illustrates the major health conditions affecting adults aged 70 and over in Cumbria, measured in Disability-Adjusted Life Years (DALYs), a metric that captures both premature mortality and years lived with disability. Larger rectangles indicate a greater disease burden, with different colours representing distinct categories of illness.
Cardiovascular diseases, particularly heart disease and strokes, account for the greatest proportion of health loss in older adults, followed closely by cancers. Lung diseases, including chronic obstructive pulmonary disease (COPD) and respiratory infections, are also significant contributors. Musculoskeletal conditions such as arthritis and osteoporosis impact mobility and independence, while diabetes, kidney disease, dementia, and mental health disorders contribute to long-term disability. Hearing and vision impairment, digestive issues, and chronic lung diseases are present but have a smaller impact.
Falls and injuries remain a concern, particularly in those with frailty, though their contribution to overall disease burden is lower than that of chronic illnesses. These patterns highlight the importance of preventative care, mobility support, and fall prevention strategies to promote independence and reduce hospital admissions.
Chronic Diseases and Multimorbidity
Older adults in Cumberland commonly experience a range of chronic health conditions, which often co-exist, leading to multimorbidity and more complex healthcare needs.
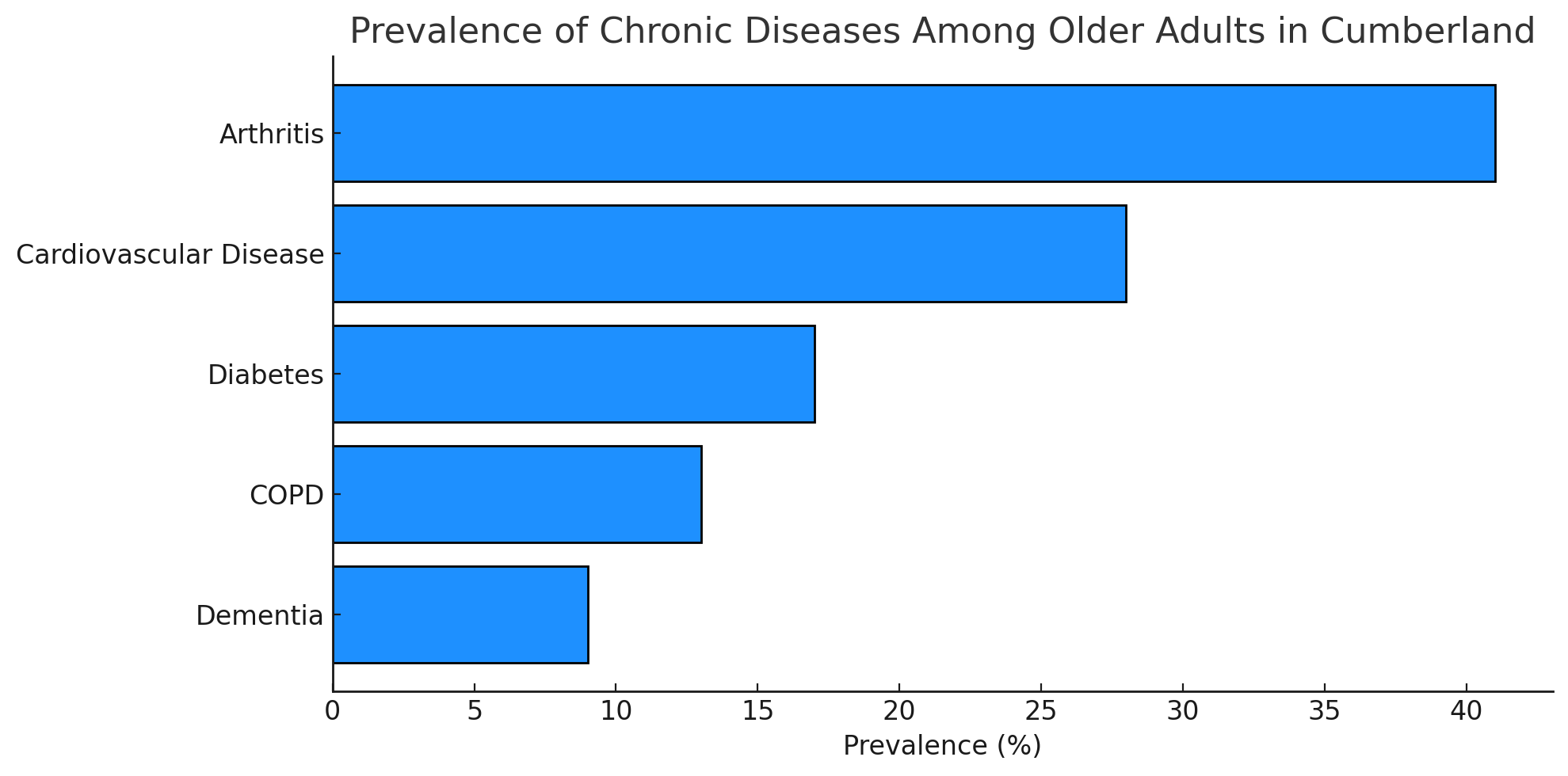
Figure 7: Prevalence of Chronic Diseases Among Older Adults in Cumberland (2023)
Source: Compiled from NHS Digital, British Geriatrics Society, and Alzheimer's Society, 2023.
The most prevalent conditions include:
- Cardiovascular Disease (CVD): Approximately 28% of older adults in Cumberland are affected, with high rates of hypertension and heart disease (NHS Digital, 2023).
- Diabetes: Affecting around 18% of those aged 65 and over, diabetes significantly increases the risk of complications such as neuropathy and kidney disease (NHS Digital, 2023).
- Chronic Obstructive Pulmonary Disease (COPD): With a 12% prevalence, COPD is a leading cause of hospitalisation in older adults.
- Arthritis and Musculoskeletal Conditions: Over 40% of older adults report joint pain or mobility issues due to osteoarthritis and rheumatoid arthritis (British Geriatrics Society, 2023).
- Dementia: Approximately 9% of Cumberland’s older population has dementia, with a projected 25% increase in cases by 2035 (Alzheimer’s Society, 2023).
Frailty and Its Impact on Healthcare Demand
Frailty is a major concern among Cumberland’s older adults, particularly those over 80, leading to increased hospital admissions, care dependency, and loss of independence. Defined as a condition where minor health issues can trigger severe declines in health, frailty is becoming more prevalent as the population ages (British Geriatrics Society, 2023).
Physical inactivity accelerates muscle loss, increasing the risk of falls and fractures. Many older adults also experience polypharmacy, where taking multiple medications can lead to side effects, drug interactions, and a higher likelihood of falls (NICE, 2023). Malnutrition, particularly in those living alone or in deprived areas, contributes to weight loss and frailty progression. Additionally, cognitive decline, including dementia and depression, exacerbates frailty and makes self-care increasingly difficult.
Mental Health and Social Isolation
Mental health plays a crucial role in overall well-being, yet conditions such as depression and anxiety often go unrecognised in older adults. Nearly 20% of older residents experience these conditions, which are frequently linked to bereavement, social isolation, and chronic illness (Age UK, 2022).
Dementia rates continue to rise, particularly in those aged 80 and over, placing increasing strain on both healthcare services and family caregivers. Social isolation is another pressing issue, particularly in rural areas, where limited transport and fewer community services contribute to loneliness and poorer health outcomes (Cumberland Council, 2023).
Social Determinants of Health
Older adults in Cumberland face several social determinants that significantly impact their health:
- Income and Poverty: Around 18% of elderly residents live in relative poverty, affecting their ability to afford nutritious food, home heating, and healthcare services (Joseph Rowntree Foundation, 2023).
- Housing Conditions: Older housing stock in rural areas often lacks age-friendly adaptations, making independent living more challenging.
- Transportation Barriers: Limited public transport options in rural areas restrict access to healthcare services, social activities, and essential amenities.
- Access to Healthcare: Rural health inequalities mean that older adults in remote areas face delays in receiving medical attention, leading to poorer health outcomes.
Potential Implications of These Trends
The decline in Healthy Life Expectancy in Cumberland raises significant concerns for healthy ageing policies. As more people spend a greater proportion of their later years in poor health, demand for healthcare, social care, and community support will rise. This challenge is particularly acute in rural areas where services are less accessible.
As Cumberland’s population continues to age, several key challenges are anticipated:
- Increased Demand for Services – Health and social care provision will need to expand, particularly for long-term care, palliative care, and chronic disease management. Greater service coverage will be required in rural areas to meet rising demand.
- Workforce Strain – The health and social care workforce will need to grow and adapt, ensuring there are sufficient trained professionals to support older adults with complex health needs (The King’s Fund, 2023).
- Economic Impact – A larger ageing population will place greater financial strain on public services, necessitating careful allocation of resources to address evolving priorities.
- Social Isolation Risks – Older adults, particularly in rural communities, are at heightened risk of loneliness and social exclusion due to limited transport, fewer local support networks, and restricted access to essential services (Age UK, 2022).
Addressing These Challenges Through Prevention
To reduce the impact of these trends, a stronger emphasis on preventative interventions is essential. Ensuring that older adults remain independent and maintain a good quality of life for longer will help relieve pressure on health and social care services.
Key areas for action include:
- Early diagnosis and better management of chronic conditions, helping older people to stay healthier for longer.
- Expanding access to physical and social activity programmes, promoting mobility, social engagement, and mental well-being.
- Reducing health inequalities through targeted local policies and investment in social care infrastructure, particularly in rural areas.
By prioritising prevention and early intervention, Cumberland can support healthy ageing, reduce pressure on care services, and create a more sustainable and equitable health system for future generations.
Chapter 2: Building an Age-Friendly Cumberland: A Framework for Healthy Ageing
Chapter 2: Building an Age-Friendly Cumberland: A Framework for Healthy AgeingCreating age-friendly communities is essential to promoting healthy ageing and ensuring that older adults remain active, engaged, and socially included. The World Health Organization’s (WHO) Age-Friendly Cities and Communities framework provides a comprehensive approach to designing environments that support physical, social, and economic participation at all stages of life (WHO, 2024). Cumberland has embraced this framework, aligning its initiatives with the eight key domains of action outlined by the WHO. These domains ensure that ageing populations can maintain independence, access essential services, and actively engage in their communities.
The Eight Domains of Age-Friendly Communities
The WHO’s framework highlights eight interconnected domains that contribute to creating inclusive, supportive environments for older adults. These domains are:
Outdoor Spaces and Buildings: Ensuring that public spaces, parks, and buildings are accessible, safe, and welcoming for older adults.
Transportation: Providing affordable, reliable, and accessible transport options to enable older adults to move around independently.
Housing: Offering a range of housing options that are affordable, adaptable, and suitable for ageing in place.
Social Participation: Encouraging older adults to engage in social, cultural, and recreational activities to reduce isolation and promote well-being.
Respect and Social Inclusion: Fostering a culture of respect and inclusion for older adults, ensuring they feel valued and integrated into community life.
Civic Participation and Employment: Supporting older adults to remain active in the workforce or volunteer sectors, contributing their skills and experience.
Communication and Information: Ensuring that information is accessible and easy to understand, particularly for those with sensory or cognitive impairments.
Community Support and Health Services: Providing accessible, high-quality health and social care services tailored to the needs of older adults.
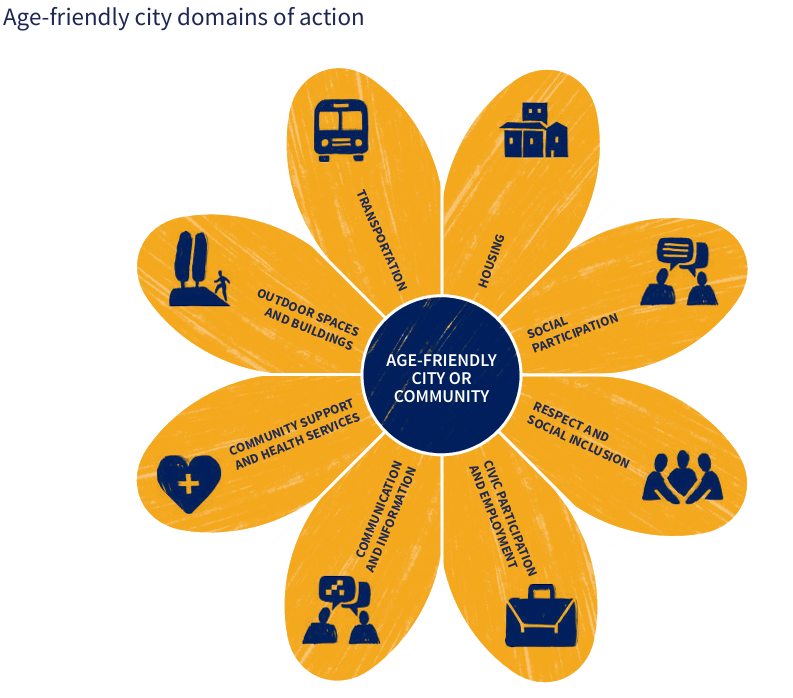
Figure 8: WHO Age-Friendly City Domains of Action
Source: World Health Organization (WHO), Age-Friendly Cities Framework.
These domains are not standalone; they are interconnected, and progress in one area often supports improvements in others. For example, accessible transportation enables older adults to participate in social activities, while inclusive housing supports their ability to live independently.
Cumberland's Age-Friendly Initiatives
Cumberland has taken significant steps towards becoming an age-friendly community, aligning its policies and initiatives with the WHO framework. Key initiatives include:
The Cumberland Age-Friendly Board: Established to drive policy and initiatives that improve housing, transport, healthcare, and social inclusion for older adults (Cumberland Council, 2024).
Age-Friendly Partnership Groups: Working in Carlisle and West Cumberland to engage older residents in shaping local services and promoting inclusivity.
Community-Based Support Networks: Expanding initiatives like befriending programmes, social clubs, and volunteer networks to combat loneliness and ensure older adults feel valued within their communities.
These initiatives reflect Cumberland’s commitment to creating an environment where older adults can thrive. By addressing the eight domains of the WHO framework, Cumberland is working to ensure that public spaces, services, and infrastructure cater to the needs of an ageing population, promoting well-being, independence, and social connectivity.
The Role of Age-Friendly Communities in Healthy Ageing
Age-friendly communities play a crucial role in supporting healthy ageing. By addressing the social determinants of health, such as housing, transport, and social inclusion, these communities help reduce the risk of frailty, social isolation, and poor health outcomes. For example, accessible outdoor spaces and buildings encourage physical activity, which is essential for maintaining mobility and reducing the risk of falls (de Labra et al., 2015). Similarly, social participation and community support networks help combat loneliness, which is a significant risk factor for mental health issues and frailty (Walsh et al., 2023).
Cumberland’s efforts to build age-friendly communities are already showing positive effects. Initiatives like the Live Longer Better in Cumbria programme, which promotes physical activity and social engagement, are helping older adults stay active and connected (Active Cumbria, 2024). Similarly, the integration of health and social care services through initiatives like Carlisle Healthcare’s Elderly Care Services ensures that older adults receive holistic support tailored to their needs (Carlisle Healthcare, 2024).
Moving Forward: Embedding Age-Friendly Principles
To further embed age-friendly principles into its policies and practices, Cumberland must continue to prioritise the following:
Engaging Older Adults: Ensuring that older residents are actively involved in decision-making processes, from planning to implementation.
Addressing Inequalities: Targeting resources towards deprived and rural areas where older adults face greater barriers to accessing services.
Collaborating Across Sectors: Strengthening partnerships between local authorities, healthcare providers, and third-sector organisations to deliver integrated, age-friendly services.
Monitoring Progress: Regularly evaluating the impact of age-friendly initiatives to ensure they are meeting the needs of older adults.
By adopting a holistic, age-friendly approach, Cumberland can create a more inclusive and supportive environment for its ageing population, ensuring that older residents can lead fulfilling, active, and socially engaged lives.
Chapter 3: Social Inclusion
Chapter 3: Social InclusionSocial inclusion is a critical aspect of healthy ageing, ensuring that older adults can actively participate in society, maintain social connections, and access essential services. In Cumberland, an ageing population, rural isolation, and economic inequalities contribute to barriers that limit social engagement for many older residents. Addressing these challenges requires targeted interventions to enhance community participation, improve accessibility, and reduce social isolation.
Barriers to Social Inclusion in Cumberland
A 2022 report by Age UK Carlisle & Eden highlighted three major issues for older adults in Cumberland: transport, social interaction, and accessibility. Of these, transport was the biggest concern, with over a quarter of respondents (25.3%) saying that limited, expensive, or inaccessible transport options prevented them from taking part in social activities (Age UK Carlisle & Eden, 2022). Many older adults rely on buses or taxis to reach essential services, but limited availability, high costs, and inaccessible transport for those with mobility issues create significant barriers. The report highlights that many respondents, particularly in rural areas, struggle to access medical appointments, community centres, and shopping facilities, increasing the risk of isolation and reduced independence.
Social interaction was another key theme, with 13.6% of respondents stating that they needed more opportunities for social engagement (Age UK Carlisle & Eden, 2022). Many requested more social groups, lunch clubs, men’s groups, and informal gatherings to help combat loneliness. However, barriers such as lack of transport, anxiety, and an unwelcoming community atmosphere often discouraged participation. The cost of attending social events was also highlighted as a concern, particularly for those on lower incomes.
Additionally, ageism and lack of respect from younger generations were cited as barriers to inclusion. 12.6% of respondents noted that they often felt overlooked, dismissed, or treated with impatience, particularly when experiencing mobility or cognitive difficulties (Age UK Carlisle & Eden, 2022). These issues were particularly pronounced in urban areas, where fast-paced environments can make older adults feel excluded from public life. Many participants emphasised that a truly age-friendly community should foster greater respect, patience, and understanding across generations.
Geographic and Rural Challenges
Cumberland’s demographic and geographic characteristics present unique challenges to social inclusion. The region includes 14 key service centres, such as Carlisle, Whitehaven, and Cockermouth, which act as hubs for public services and community engagement. However, older adults living in smaller villages and remote rural areas often struggle with limited transport options and reduced access to healthcare, shops, and social spaces (Cumberland Council, 2023). Rural isolation is a well-documented issue affecting older adults, leading to higher rates of loneliness, mental health concerns, and difficulty accessing support networks (Public Health England, 2020).
Strategies to Improve Social Inclusion
To create an age-friendly Cumberland, targeted interventions should focus on enhancing social participation, improving accessibility, and fostering intergenerational relationships. Key recommendations include:
- Expanding Rural Transport Services: Improved public transport options, including community buses and subsidised taxi schemes, would enable older adults to reach essential services and social activities more easily.
- Developing Age-Friendly Community Hubs: Establishing multi-purpose community spaces in towns and villages could provide social, educational, and recreational activities tailored to older adults.
- Encouraging Intergenerational Engagement: Promoting volunteering programs, mentorship schemes, and joint community projects can help bridge the gap between younger and older generations, fostering mutual respect and understanding.
- Enhancing Accessibility and Digital Inclusion: Many older adults in Cumberland face barriers to digital access, limiting their ability to connect with services and social networks. Providing digital literacy programs alongside non-digital communication options (e.g., newsletters, phone support) would help reduce exclusion.
- Promoting Affordable Social Activities: Community groups, councils, and charities should offer low-cost or free activities, ensuring that financial constraints do not prevent older residents from engaging with their communities.
Chapter 4: Digital Health and Literacy
Chapter 4: Digital Health and LiteracyDigital health literacy, defined as the ability to seek, understand, and use health-related information from electronic sources, is becoming increasingly vital for older adults to manage their health effectively. In Cumberland, improving digital health literacy among the ageing population is essential to ensure equitable access to healthcare resources, telehealth services, and online health information.
Research highlights that digital health literacy interventions can significantly improve knowledge, confidence, and engagement with online health resources, though practical skills development may require more targeted support (Zhao et al, 2022). Factors influencing digital health literacy include age, education level, access to digital devices, and availability of social support networks, all of which determine an individual’s ability to engage with digital healthcare tools effectively (Grüning et al, 2023). Addressing these barriers through structured interventions and accessible digital health resources is critical in enabling older adults to navigate the digital healthcare landscape independently.
Barriers to Digital Literacy in Cumberland
Older adults in Cumberland face several challenges that hinder their engagement with digital health services. Digital exclusion is a key issue, particularly in rural areas where internet access is limited, and older adults may have fewer opportunities for digital literacy training (Cumberland Council, 2023). Many older residents also struggle with accessing online GP services, ordering prescriptions digitally, or using wearable health technology, creating disparities in healthcare access and self-management (Public Health England, 2021).
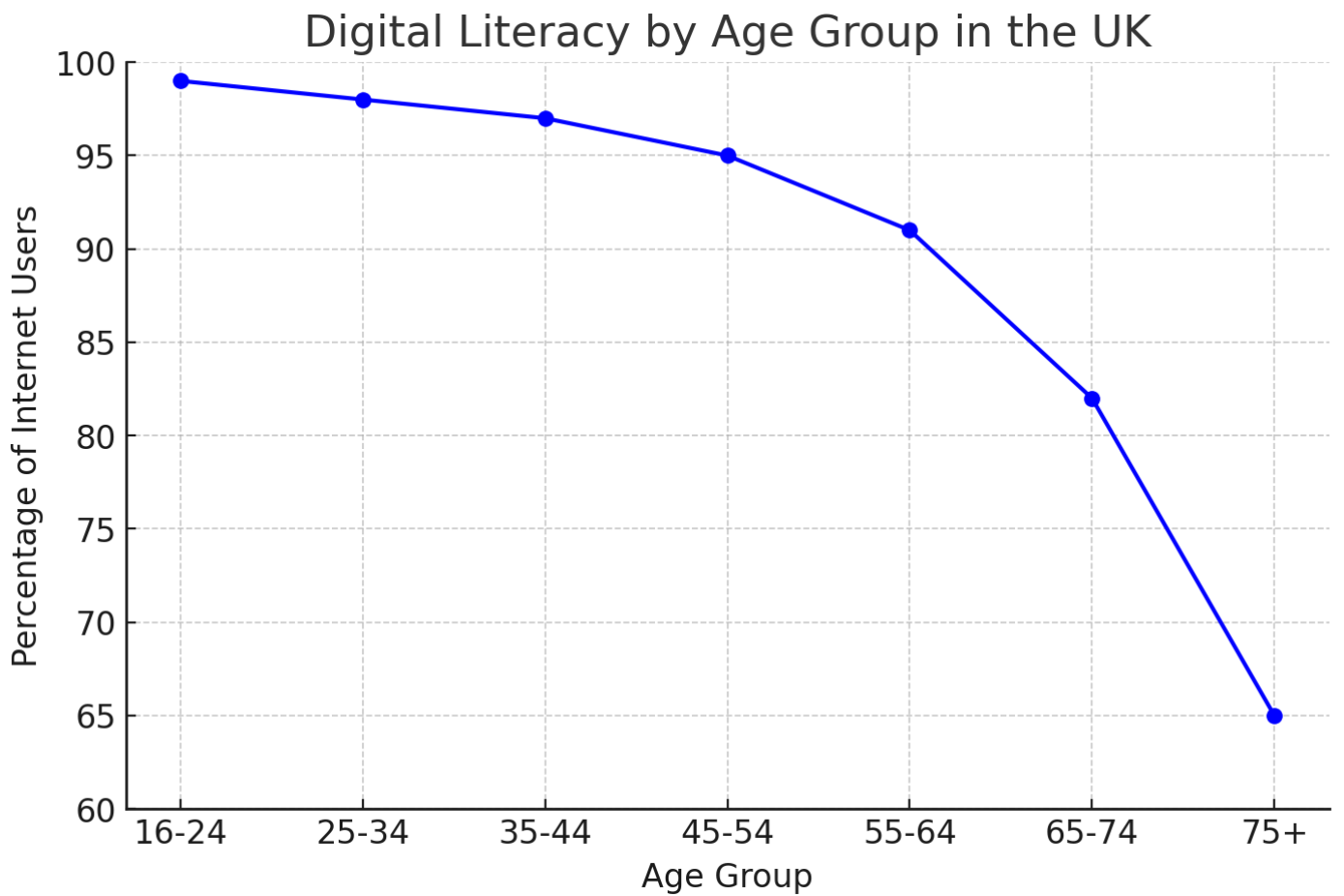
Figure 9: Digital Literacy by Age Group in the UK
Source: Office for National Statistics (ONS), Internet Access – Households and Individuals, 2023
National data (figure 9) indicates that while internet usage is high among younger age groups, there is a notable decline among those aged 65 and over. This trend suggests that older adults may face challenges related to digital literacy, which could impact their ability to access online health resources effectively. This will need to be addressed as we become more reliant on technology and healthcare services continue to become more digitised.
Many older adults are hesitant to use digital health platforms due to concerns about privacy, security, and the reliability of online health advice. Building trust in these tools is key to increasing their adoption (Zhao et al, 2022). These issues are exacerbated by economic barriers, as some older residents may lack the financial resources to afford smartphones, tablets, or reliable broadband connections (Cumberland Council, 2023).
Digital tools, such as the NHS App, have the potential to make healthcare more accessible, but not everyone can use them easily. Many older adults face challenges with digital literacy and relying too heavily on online services risks leaving some people behind. A balanced approach, one that maintains phone and in-person options alongside digital tools, will be essential.
The NHS App enables users to book GP appointments, order prescriptions, and access their health records, yet evidence suggests that uptake among older adults remains low, with barriers including lack of digital confidence, concerns about data security, and difficulty navigating the interface (Palmer et al., 2023). Additionally, studies indicate that digital health interventions must be accompanied by human support mechanisms to be effective, as many older adults benefit from guided learning rather than self-directed app use (Watson et al., 2022). Over-reliance on the NHS App as a primary route for healthcare access may therefore widen health inequalities rather than reduce them, particularly in rural areas like Cumberland where digital infrastructure is inconsistent. A more balanced approach is needed, integrating face-to-face, telephone, and digital services to ensure that technology complements rather than replaces traditional healthcare pathways (Greenhalgh et al., 2023).
Initiatives to Improve Digital Health Literacy in Cumberland
To bridge the digital divide and improve digital health literacy among older adults, Cumberland has implemented several initiatives. However, ongoing efforts are required to ensure digital solutions are accessible, inclusive, and do not replace traditional healthcare access routes. The following strategies combine current initiatives with recommendations for future improvements to create a more sustainable and effective approach.
- Cumberland Digital Inclusion Programme: Cumberland Council has launched community-based digital literacy training for older adults, covering NHS online services, digital prescriptions, and GP appointment booking via NHS apps.
🔹 Future Action: Expand training to include alternative healthcare access options (e.g., telephone services) and focus on guided, long-term digital support rather than one-off sessions. - Broadband Expansion in Rural Areas: Recognising digital infrastructure challenges, Cumberland Council is working with government initiatives to expand high-speed broadband access in rural areas.
🔹 Future Action: Ensure broadband expansion is complemented by affordable internet access schemes and offline service options for those who remain digitally excluded. - Library-Based Digital Literacy Support: Public libraries now provide one-on-one digital health support, assisting older adults with NHS websites, video consultations, and navigating health apps.
🔹 Future Action: Implement trained staff in GP surgeries and libraries who can offer on-demand, ongoing digital support rather than ad-hoc sessions. - Community-Led Support Networks: Charities, including Age UK Carlisle & Eden, offer peer-led digital skills workshops to help older adults gain confidence using smartphones, health apps, and wearable technology.
🔹 Future Action: Shift focus beyond basic digital skills to include more advanced skills, in order to help older adults better access online health information and build trust in digital platforms. - Maintaining Hybrid Healthcare Access: Recognising concerns about over-reliance on the NHS App, Cumberland is committed to ensuring digital tools complement rather than replace face-to-face and telephone healthcare services.
🔹 Future Action: Advocate for local NHS services to maintain non-digital appointment booking, ensuring that older adults have multiple access points to care.
By fostering digital health literacy through these community-driven and technology-inclusive initiatives, Cumberland is taking steps to ensure older residents can access healthcare information, communicate with providers, and manage their health independently
Chapter 5: Housing
Chapter 5: HousingHaving a safe and accessible home is essential for healthy ageing. For older adults in Cumberland, well-designed housing can prevent ill health, reduce social isolation, and support independent living. As the number of people aged 65 and over continues to grow, housing policies and developments must proactively address affordability, accessibility, and integration with social care services.
Housing Needs for Older Adults in Cumberland
Older residents often require housing that meets their changing mobility and health needs, yet many existing homes lack the necessary adaptations for safe and independent living. Additionally, fuel poverty and energy inefficiency are key concerns, particularly in rural and older housing, which contributes to excess winter deaths and cold-related illnesses (National Energy Action, 2023).
To meet these needs, Cumberland must ensure that housing options and policies align with both local priorities and national housing targets.
National House-Building Targets and Local Planning
The UK Government has committed to delivering 1.5 million new homes by 2029, with an annual target of 300,000 homes to address the national housing shortage (Department for Levelling Up, Housing and Communities, 2023). However, current completion rates remain below target, with only 193,000 homes built in 2023 (Reuters, 2024).
A key challenge will be ensuring that new housing is not only built but designed to meet the specific needs of older people, including accessibility features, integration with healthcare services, and sustainable energy efficiency measures.
Housing Options for Older Adults in Cumberland
Cumberland offers a range of housing options designed to support older adults at different levels of independence and care needs:
- Extra Care Housing – These self-contained, accessible homes cater to individuals over 55 who require some level of support while maintaining independence. With on-site care services and age-friendly adaptations, these settings provide security while enabling autonomy (Cumberland Council, 2023).
- Sheltered Housing – Consisting of self-contained flats with emergency alarm systems and access to support staff, sheltered housing enhances safety, social interaction, and mental well-being by reducing loneliness and fostering community engagement (Cumberland Council, 2023).
- Residential Care Homes – For older adults requiring round-the-clock assistance, Cumberland offers residential care facilities, including specialised dementia care units. These homes support individuals with complex needs in a safe and professional environment (Care Quality Commission, 2022).
Key Challenges in Housing Older Adults
Despite existing provisions, several challenges hinder older adults from accessing appropriate housing:
1. Affordability and Accessibility
Many older adults in Cumberland face difficulties finding housing that is both affordable and suitable for their needs. Rising housing costs, particularly in the private rental sector, make it harder for those on fixed pensions to relocate to more accessible accommodation (Cumberland Council, 2023). Limited availability of affordable age-friendly housing means that many older residents remain in homes that no longer meet their needs, increasing the risk of falls and hospital admissions (Public Health England, 2021).
Even when older adults want to adapt their homes to support independent living, the cost of essential modifications, such as stairlifts, handrails, and accessible bathrooms, can be prohibitive. While government schemes like the Great British Insulation Scheme offer financial support for energy efficiency improvements, awareness remains low, and many older people miss out on these benefits (Department for Energy Security and Net Zero, 2023). Local authorities have a key role in raising awareness and streamlining access to home adaptation grants and retrofitting programmes, ensuring more residents can safely age in place.
2. Affordable Warmth and Energy Efficiency
For many older adults in Cumberland, keeping their homes warm throughout the winter is a constant struggle. Fuel poverty remains a pressing issue, particularly in older, poorly insulated homes where high heating costs force many residents to choose between warming their home or meeting other essential expenses.
The consequences of cold homes extend beyond discomfort—they contribute to serious health risks, including respiratory illnesses, cardiovascular conditions, and excess winter deaths (National Energy Action, 2023). Vulnerable individuals, especially those with pre-existing health conditions, face a heightened risk of hospitalisation due to prolonged exposure to cold temperatures.
Government initiatives, such as the Great British Insulation Scheme, aim to improve energy efficiency and reduce heating costs, offering support for home insulation and heating upgrades (Department for Energy Security and Net Zero, 2023). However, awareness and uptake of these schemes remain low among older and vulnerable populations, meaning many who would benefit most from subsidised home improvements are missing out.
3. Integration with Social Care Services
For many older adults in Cumberland, accessing the right support within their housing setting can be a frustrating and complex process. While services exist to assist with health, personal care, and daily living needs, many older residents struggle to navigate the system, often only receiving help when their situation reaches a crisis point.
A major barrier is the lack of coordination between housing, social care, and health services, which leaves many older adults without the preventative support they need to remain independent for longer (Public Health England, 2021). Without proactive interventions, minor issues—such as mobility challenges or managing long-term health conditions—can escalate into avoidable hospital admissions or the need for emergency care.
Future Considerations for Housing in Cumberland
To address these challenges and improve housing for older adults, the following strategies should be prioritised:
Expansion of Affordable Age-Friendly Housing
As Cumberland works towards meeting national house-building targets, it is essential to prioritise affordable, purpose-built housing designed to meet the needs of older residents. Housing policies should encourage investment in mixed-tenure developments, ensuring a balance of social, rental, and ownership options. By creating housing that is adaptable and suitable for ageing in place, older adults can maintain their independence for longer while benefiting from secure and accessible living environments.
Retrofitting Homes for Accessibility and Energy Efficiency
Increasing funding for home adaptations, such as grab rails, stairlifts, and accessible bathrooms, will allow more older residents to continue living safely in their own homes. Expanding access to affordable warmth schemes, including insulation grants and fuel subsidies, can also help reduce cold-related health risks. Local authorities have a key role to play in raising awareness of government initiatives, such as the Great British Insulation Scheme, to ensure that older adults benefit from available support for energy efficiency improvements.
Integrating Housing with Social Care Services
Cumberland Council has already brought its housing and adult social care services into one team. A more coordinated approach between housing providers, NHS services, and social care teams will help older adults receive the support they need to live independently at home. Digital solutions, such as remote monitoring and telecare, can provide reassurance and medical support while allowing residents to maintain their autonomy. Exploring multi-generational housing developments could also provide alternative solutions, fostering intergenerational support networks and reducing social isolation among older adults.
By implementing these measures, Cumberland can ensure that its ageing population has access to safe, affordable, and well-supported housing, ultimately improving health outcomes and quality of life for older residents.
Chapter 6: Supporting Older Adult Health in Cumberland
Chapter 6: Supporting Older Adult Health in CumberlandCumberland is home to a wide range of services and initiatives aimed at promoting and improving the health and well-being of older adults. These services, provided by both statutory and third-sector organisations, play a crucial role in preventing social isolation, enhancing mobility, and ensuring access to essential healthcare and support systems. However, despite the breadth of services available, significant challenges remain. Rising demand, workforce shortages, and resource constraints are putting increasing pressure on service providers. Moreover, a small proportion of the population accounts for a large share of service provision, highlighting the need for a more radical and proactive approach to supporting older adults, particularly those managing frailty and multiple long-term conditions.
This chapter outlines the key services and initiatives in Cumberland that support older adults, with a particular focus on frailty management and healthy ageing. It also explores the challenges faced by these services and the innovative approaches being adopted to address them.
Community Support and Health Services
Cumberland offers a variety of community support and health services designed to help older adults live independently and maintain their health and well-being. These services are essential in reducing social isolation, enhancing physical health, and providing holistic healthcare support. Below are some key examples of these services:
Figure 10: Community support service for older adults
Frailty and Healthy Ageing
Frailty is often misunderstood. It is not simply an unavoidable part of getting older but a condition where the body gradually loses its ability to recover from illness, injury, or even everyday stresses. Some people remain active and independent well into their nineties, while others find themselves struggling much earlier. When frailty is poorly managed, even a minor infection or a small fall can result in significant loss of independence, hospitalisation, or long-term care.
However, frailty is not inevitable, nor does it have to mean a loss of quality of life. With the right preventative care, early identification, and tailored support, many older adults can continue to live well for longer. Cumberland is working towards a proactive, community-based approach to frailty that focuses on prevention, early intervention, and better integration between health and social care services.
The Growing Challenge of Frailty in Cumberland
As Cumberland’s population ages, frailty is becoming an increasingly urgent public health concern. National data shows that the prevalence of frailty is rising, reflecting broader demographic shifts in the UK. However, frailty is not just linked to ageing, it is heavily influenced by social and economic factors.
Recent local data from North Cumbria Integrated Care (NCIC) NHS Foundation Trust reinforces the scale of this challenge. Between 2022 and 2024, the number of hospital admissions for older adults (aged 65 and over) with frailty-related conditions increased by 33%, rising from 1,591 to 2,113 (Table 4). These figures reflect a growing burden on acute services and underscore the importance of preventative, community-based approaches to frailty.
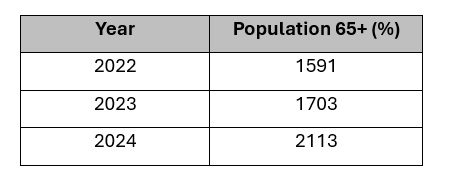
Table 4: Hospital Admissions for 65+ Patients with Frailty-Related ICD-10 Codes
Source: North Cumbria Integrated Care NHS Foundation Trust, 2025.
Alongside this, the proportion of older adults arriving in hospital with a Clinical Frailty Score (CFS) of 6 or more, indicating moderate to severe frailty, has been increasing over the past year. By January 2025, nearly one in three older patients (31.8%) fell into this category, up from 25.7% in March 2024 (Figure 11). This rising trend highlights the need for earlier identification and community-based support to reduce avoidable admissions and improve outcomes.
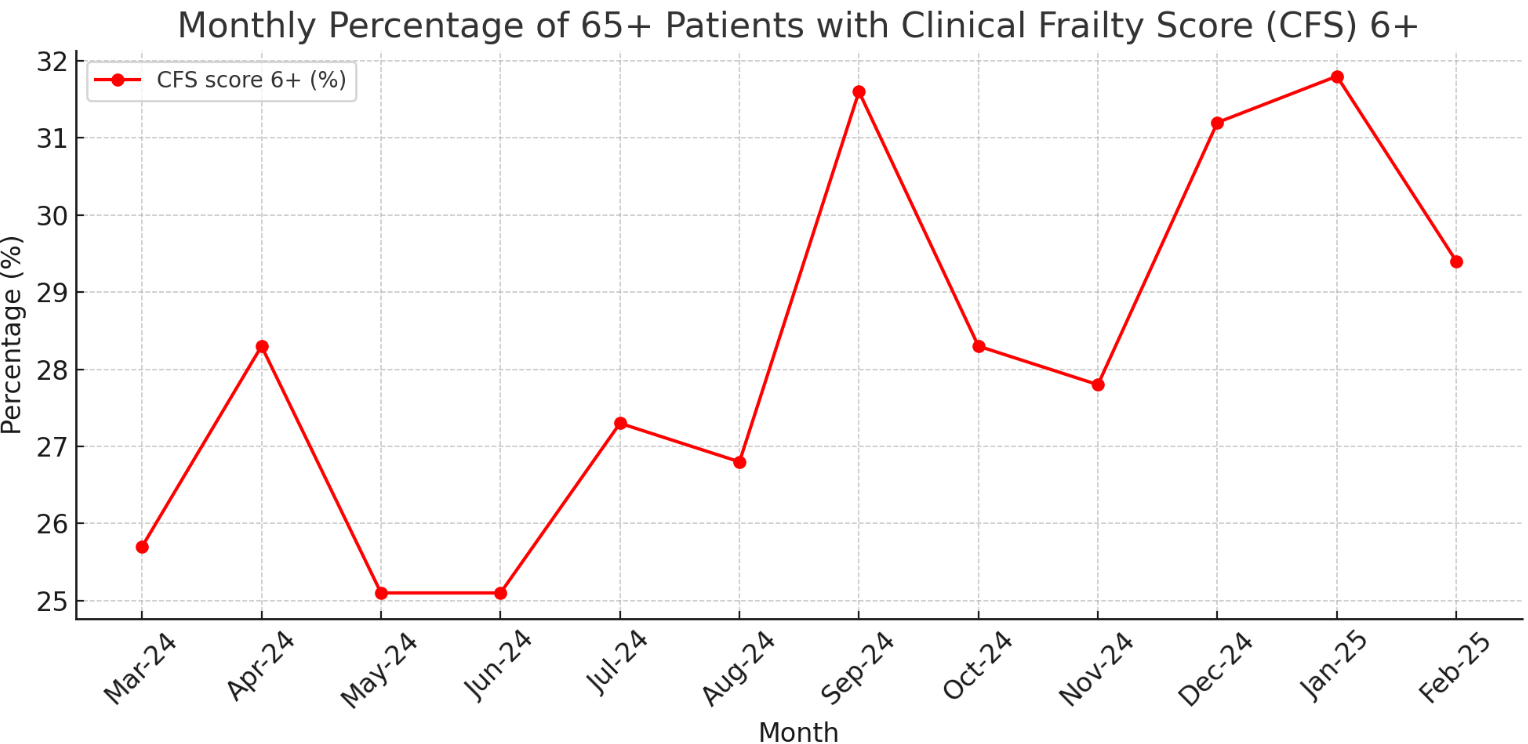
Figure 11: Monthly percentage of patients aged 65 and over with a Clinical Frailty Score (CFS) of 6 or above (March 2024 – February 2025)
Source: North Cumbria Integrated Care NHS Foundation Trust, 2025.
In addition, frailty score data collected over the past 104 weeks shows that fewer than 6% of older adults admitted to hospital were classified as ‘Very Fit’, while nearly half were recorded as mildly, moderately, or severely frail (Figure 12). These insights provide a valuable foundation for targeting interventions at those most at risk and for planning services around the needs of an ageing, increasingly frail population.
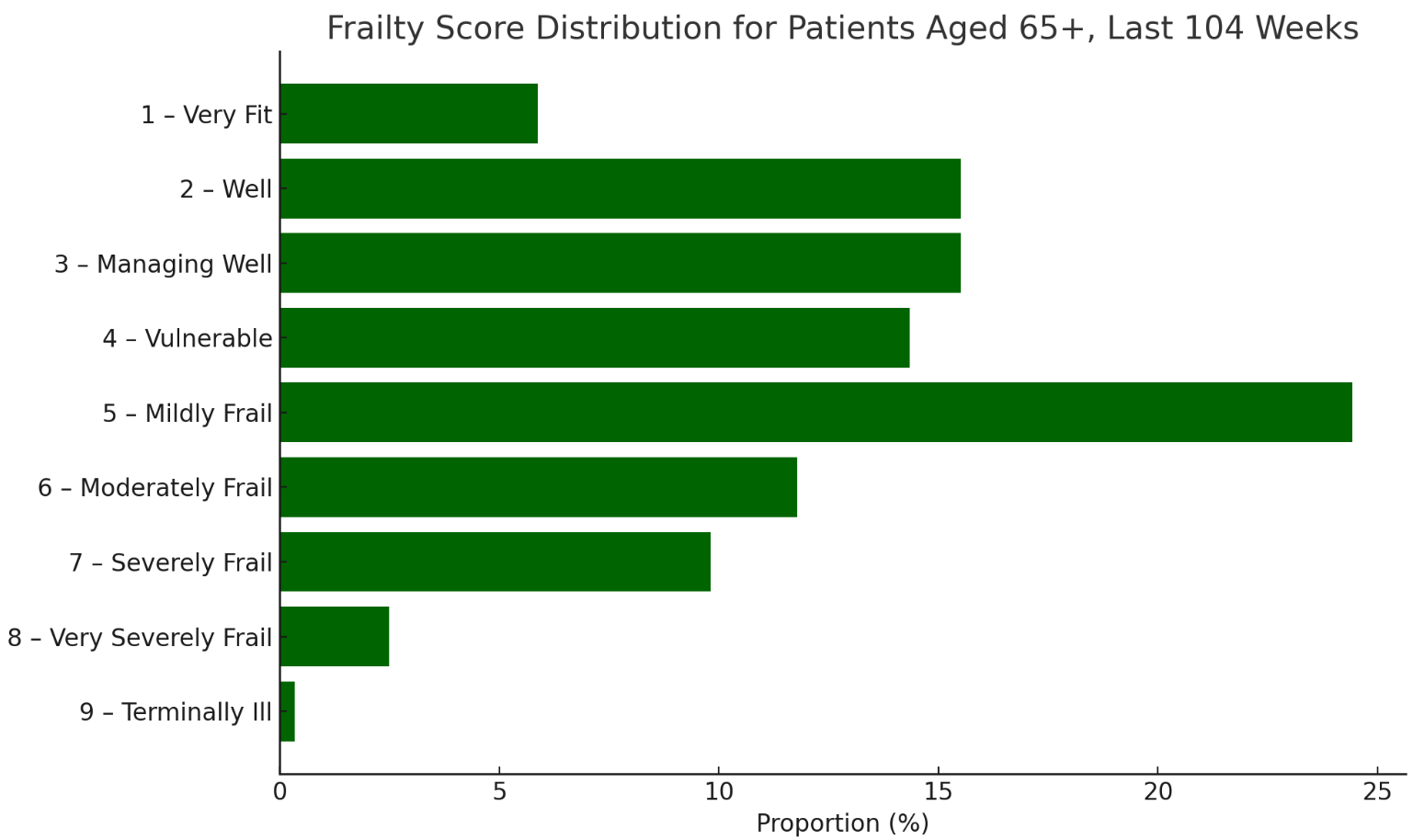
Figure 12: Frailty score distribution among patients aged 65 and over admitted to hospital, based on Clinical Frailty Scores recorded over the past 104 weeks
Source: North Cumbria Integrated Care NHS Foundation Trust, 2025.
Research indicates that individuals in deprived areas are twice as likely to experience frailty compared to those in more affluent communities (Sinclair et al., 2021). This pattern is reflected in Cumberland’s Primary Care Network (PCN) data, which highlights significant variations in frailty prevalence across different localities. People living in rural areas, those with long-term conditions, and individuals experiencing social isolation are at the greatest risk of developing frailty (Walsh et al., 2023).
Understanding these inequalities is essential in designing targeted interventions that address the needs of those most at risk. The approach taken in Cumberland is based on five key ambitions, aligning with the North Cumbria Frailty Strategy (2025-2029). These ambitions provide a structured framework for ensuring that older adults receive the right care, at the right time, in the right place (North Cumbria Place-Based Partnership, 2025).
1. Preventing Well: Staying Stronger for Longer
Frailty does not develop overnight, it is the result of gradual changes such as muscle loss, reduced mobility, poor nutrition, and social isolation. Without intervention, these small declines can lead to serious health deterioration. However, when caught early, frailty can be delayed, slowed, or even reversed.
Preventing frailty starts with keeping active, maintaining good nutrition, and raising awareness of early risk factors. Regular strength and balance exercises reduce falls and improve mobility (de Labra et al., 2015), while nutritional support and hydration programmes help combat frailty-related malnutrition (Lorenzo-López et al., 2017). Many people do not realise they are becoming frail until a crisis occurs, so increasing public and professional awareness is essential to encourage early action.
The Proactive Care Pilot Programme (2024) in North Cumbria represents a major shift towards prevention and early intervention. Traditionally, frailty has been managed reactively, with individuals only seeking help once they are already in crisis. This programme is designed to identify at-risk individuals sooner, ensure timely support, and strengthen community-led care (Year of Care Partnerships, 2024).
By shifting the focus to prevention rather than crisis management, Cumberland aims to reduce avoidable hospital admissions and improve long-term outcomes for older adults.
2. Diagnosing Well: Identifying Frailty Before It’s Too Late
Frailty often goes undiagnosed until a serious health event occurs. However, routine screening and early diagnosis can make a significant difference in preventing deterioration and ensuring people receive timely, personalised care.
To improve early detection, expansion of routine frailty screening in GP practices and community health settings Is crucial. Comprehensive Geriatric Assessments (CGA) are also being introduced to provide a structured, personalised approach to frailty management (Briggs et al., 2022). Alongside this, digital frailty indexes are being used to track trends and identify at-risk individuals before they experience a health crisis.
By embedding frailty assessment into primary care, Cumberland is taking a preventative, rather than reactive, approach to supporting older adults.
3. Supporting Well: Building a Care System That Works for Older Adults
For those already living with frailty, the right support can mean the difference between maintaining independence and frequent hospital stays. Cumberland is working to strengthen home-based care, expand carer support, and create a more joined-up health and social care system.
One of the biggest challenges in delivering frailty care is workforce shortages, particularly in rural areas, where high vacancy rates contribute to delays in accessing care (Cumberland Council, 2023). Cumberland is working to expand frailty-specialist roles, improve recruitment in rural areas, and develop mobile care models and telehealth services to bridge gaps.
Supporting people to stay at home safely is also a priority. Expanding assistive technology, home adaptations, and falls prevention programmes allows more people to live independently for longer. Carers play a vital role in frailty care, yet many struggle with little support. Increasing respite services, carer training, and access to financial advice is crucial in ensuring that carers are not left overwhelmed.
To reduce variation in care quality, Cumberland is developing a fully integrated frailty pathway, ensuring GPs, hospitals, social care teams, and community services work together. This approach will help reduce emergency admissions and ensure that older adults receive the right support, in the right place, at the right time.
4. Living Well: Supporting Independence and Wellbeing
Frailty care is not just about managing health conditions, it is also about supporting older adults to maintain purpose, independence, and connection to their communities. Social isolation and loneliness are significant contributors to frailty, affecting both physical and mental health. Ensuring that people remain socially engaged, financially secure, and able to access community services is just as important as medical care. A detailed discussion on social inclusion, loneliness, and community-based interventions can be found in the ‘Social Inclusion’ section of this report.
5. Dying Well: Ensuring Compassionate and Dignified Care
Similarly, planning for the later stages of frailty is essential. As people approach the end of life, having clear advance care plans, good palliative care, and family support ensures that they can receive care that aligns with their wishes. Many people express a desire to be cared for at home or in a familiar setting, yet a lack of early planning often leads to hospital admissions that could have been avoided. Cumberland is working to strengthen end-of-life care services and improve coordination between healthcare providers, social services, and families. These issues are explored further in the ‘Dying Well’ section of this report.
A Future Where Frailty is Managed
Cumberland is moving away from crisis-driven frailty care towards a system that prioritises prevention, early identification, and community-based support. By embedding the five ambitions for frailty into our local strategy, we can help older adults stay healthier, more independent, and better supported.
Frailty is a challenge, however through proactive, person-centred care, we can ensure that ageing in Cumberland is not just about living longer, but living well.
Chapter 7: Dying Well and End of Life Care
Chapter 7: Dying Well and End of Life CareEnsuring individuals experience a dignified, comfortable, and well-supported end of life is a fundamental part of public health. In Cumberland, as in the rest of the UK, efforts continue to improve palliative and end-of-life care, supporting patients, families, and caregivers with high-quality, compassionate care that reflects personal preferences and needs. As the population ages, the demand for end-of-life services is increasing, necessitating a well-coordinated, multi-sector approach involving healthcare providers, social services, community organisations, and policymakers.
The North Cumbria End-of-Life Partnership (NCELP) plays a central role in shaping this approach, bringing together key stakeholders to develop a sustainable and equitable model of palliative care. This partnership ensures that Cumberland’s strategy aligns with regional priorities, with a focus on improving access, addressing health inequalities, and embedding best practice models for palliative care delivery (NCELP, 2024).
Current Landscape of End-Of-Life Care
Across the UK, many people express a preference to die at home or in a hospice, yet a significant proportion of deaths still occur in hospitals. In Cumberland, shifts in place of death trends over the past decade have been slow but noticeable.
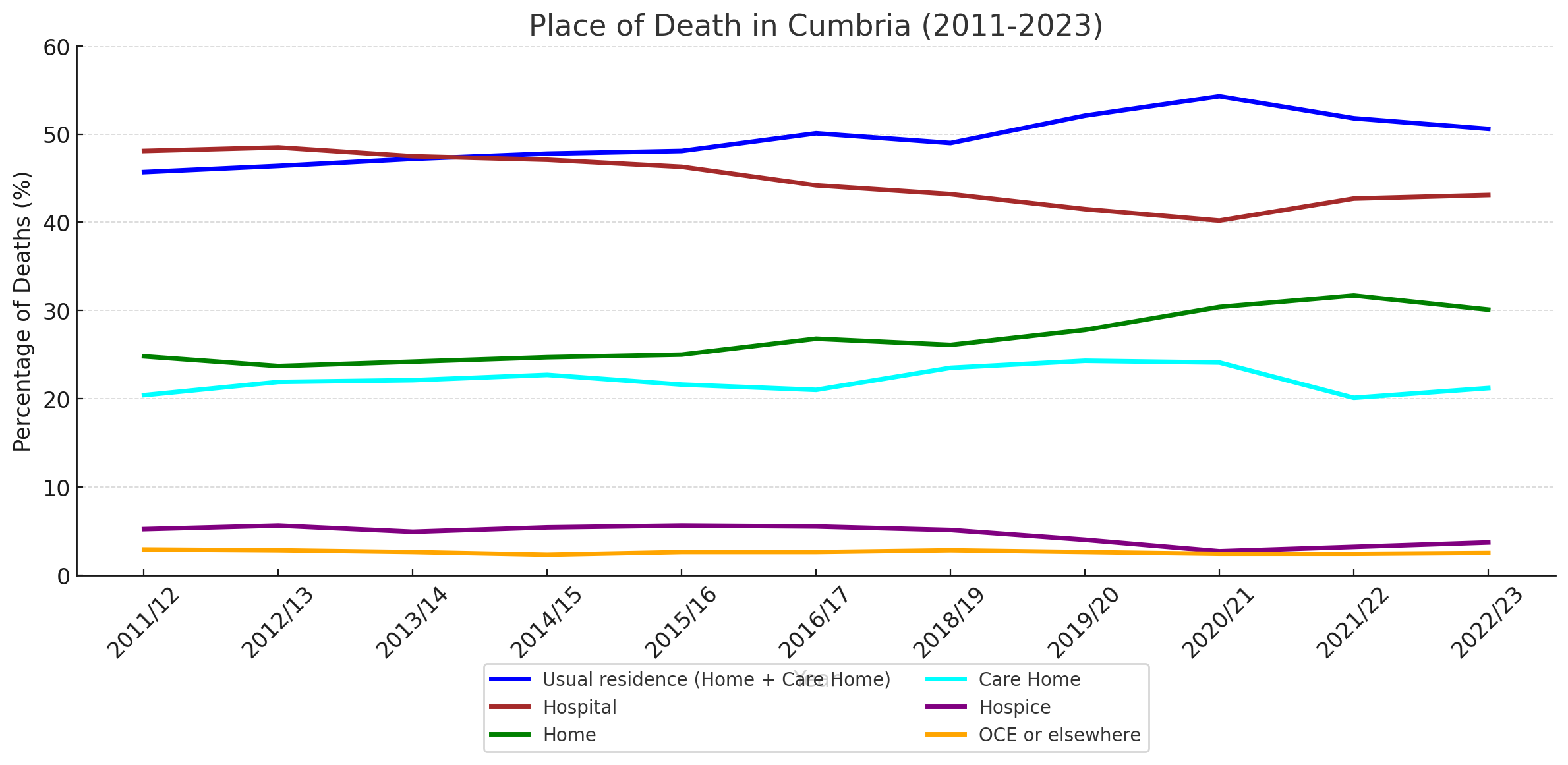
Figure 13: Summary of the Place of Death in Cumbria (2011–2023)
Source: Office for National Statistics (ONS), 2023
Figure 13 presents an overview of place of death in Cumberland from 2011 to 2023. Between 2011 and 2017, around 45% of people died in their usual residence (either at home or in a care home). By 2022/23, this had risen to just over 50%, indicating a steady increase in home-based and care home palliative care provision. Hospital deaths, while still accounting for a large proportion of deaths, have declined slightly, from nearly 50% in the early years to around 43% more recently.
Hospice deaths have remained low and stable throughout the period, consistently accounting for between 3% and 5% of total deaths. Deaths in ‘other’ settings, such as assisted living facilities or following emergency admissions, have also remained a small but consistent proportion of overall mortality.
Importantly, the combined data highlights the impact of the Covid-19 pandemic. In 2020/21, there was a marked increase in deaths occurring at home and in care homes, likely reflecting reduced hospital capacity and increased reliance on community-based care during the pandemic. While the data since then suggests a return to pre-pandemic trends, it is possible that some of the observed changes were driven by necessity rather than sustained improvements in service design or patient choice.
Overall, although it is encouraging that more people are dying in familiar settings, progress has been relatively slow. Hospitals continue to account for a significant proportion of deaths, and there remains substantial opportunity to further expand and strengthen community-based palliative and end-of-life care across Cumberland.
End-Of-Life Care Services in Cumberland
The North Cumbria Integrated Care NHS Foundation Trust (NCIC) provides a range of palliative care services for patients with life-limiting conditions. These services focus on:
- Managing pain and symptom relief.
- Providing emotional and psychological support for patients and families.
- Offering home-based palliative care to reduce unnecessary hospital admissions.
- Ensuring coordinated care planning between healthcare providers (NCIC, 2025).
NCELP has been instrumental in driving improvements in these services by fostering collaboration between primary care, hospices, and social care providers. However, delivering consistent, high-quality palliative care remains a challenge, particularly in rural areas where specialist teams may be harder to access.
Challenges in End-Of-Life Care
Disparities in Access to End-Of-Life Care
Older adults in rural Cumberland may experience limited access to specialist palliative care teams, hospice services, and community-based support, leading to an increased reliance on hospitals for end-of-life care. Ensuring that all residents have equitable access to palliative care remains a core focus of NCELP.
Workforce and Training Gaps
There is a shortage of trained palliative care professionals, including community nurses and end-of-life care coordinators. Expanding the palliative care workforce and training provision is essential to ensuring consistent, high-quality care (Kings Fund, 2023). NCELP is leading efforts to develop structured training programmes, ensuring that GPs, nurses, and social care workers are equipped to deliver compassionate, high-quality end-of-life care.
Delays in Care and Decision-Making
A lack of early discussions around advance care planning (ACP) means that some patients receive care that may not align with their preferences. Encouraging proactive ACP conversations between patients, families, and healthcare providers can help ensure greater autonomy and dignity in end-of-life decision-making.
Psychological and Emotional Support for Families
Providing bereavement support services is crucial in helping families and caregivers cope with loss and grief. Expanding specialist counselling and peer support programmes is vital to ensuring emotional well-being after the death of a loved one (NHS England, 2021).
Funding and Sustainability
One of the most pressing concerns is the financial sustainability of hospice and community-based palliative care services. Many hospices rely on charitable donations, short-term grants, and the Better Care Fund. However, without a stable funding model, these services remain vulnerable. NCELP is working with the ICB to develop long-term commissioning solutions that integrate palliative care into NHS funding streams, ensuring continuity of care for patients and families.
Policy Framework and Guidelines
End-of-life care in the UK is shaped by national frameworks and clinical guidelines that set best practices for high-quality, person-centred care.
- The National Institute for Health and Care Excellence (NICE) Guidelines NG31 outlines key principles for pain management, symptom control, and communication with families (NICE, 2015).
- Ambitions for Palliative and End-of-Life Care (2021-2026) provides a national framework for personalised, community-focused palliative care (NHS England, 2021).
- The NHS Long-Term Plan commits to expanding community-based palliative care services to allow more people to receive care in their preferred place of death (NHS England, 2022).
Cumberland is actively implementing these policies at a local level, ensuring that its palliative care services align with national ambitions for dignified, high-quality end-of-life care.
Local Initiatives in Cumberland
Expanding Community-Based Palliative Care
NCIC has been increasing palliative care services within community settings, aiming to reduce hospital deaths and ensure that patients receive holistic care closer to home (NCIC, 2025).
Hospice and Specialist End-of-Life Services
Local hospices, such as Eden Valley Hospice, continue to provide specialist palliative care, helping patients and families navigate end-of-life care with dignity (Eden Valley Hospice, 2024).
Advanced Care Planning Programmes
Efforts are being made to encourage earlier advance care planning, ensuring that patients can document their end-of-life preferences before a crisis occurs (Cumberland Council, 2024).
Bereavement and Family Support Services
Expanding grief counselling, emotional support groups, and practical bereavement guidance remains a priority, ensuring families receive the support they need (NHS England, 2021).
Advance Care Planning in Cumberland: Current Status and Opportunities for Development
Advance Care Planning (ACP) is a process that enables individuals to articulate their preferences for future medical care, ensuring that their wishes are respected even if they become unable to communicate them. Despite its importance, ACP remains under-used both nationally and within Cumberland.
Current State of Advance Care Planning in the UK
Despite the recognised importance of Advance Care Planning in ensuring that individuals' end-of-life care preferences are respected, engagement with ACP remains suboptimal across the UK. A 2013 survey by the British Medical Journal (BMJ) revealed that only 5% of British individuals had formalised an advance care plan, highlighting a significant gap in end-of-life preparedness (BMJ, 2013). Similarly, a 2017 report by Macmillan Cancer Support found that just 8% of people with cancer had discussed their end-of-life care preferences with a healthcare professional, further emphasising the lack of routine ACP discussions in clinical practice (Macmillan Cancer Support, 2017). The reluctance to engage in ACP conversations means that many end-of-life decisions are made reactively, often resulting in unwanted hospital admissions, aggressive treatments, and a reduced focus on palliative and comfort-centred care.
While ACP uptake remains low in the general population, care home residents show higher levels of engagement. A 2022 service evaluation found that 79.5% of UK care home residents had engaged in ACP, indicating that structured care environments may facilitate higher participation in advance care planning (Robinson et al., 2022). However, the study also highlighted significant inconsistencies in ACP implementation, with many care homes lacking the staffing, training, or resources to support ACP services effectively. Furthermore, gaps in communication between healthcare providers and care homes often lead to ACP preferences not being documented or honoured, undermining the intended benefits of these plans.
The data on Advance Care Planning engagement highlights a critical gap in end-of-life preparedness across the UK, with low national uptake and significant inconsistencies in implementation. The lack of routine ACP discussions means that many individuals do not have their care preferences documented, leading to reactive decision-making, increased hospital admissions, and potentially unwanted medical interventions. While ACP engagement is higher in care home settings, challenges such as staffing shortages, inadequate training, and poor communication between services limit its effectiveness.
For Cumberland, these findings reinforce the urgent need for structured ACP initiatives, including public awareness campaigns, professional training, and improved communication systems across healthcare providers. Additionally, there is a notable lack of comprehensive, up-to-date data on ACP coverage and adherence, making it difficult to assess how well ACP is integrated into healthcare systems and whether existing plans are being followed. Addressing this data gap will be crucial for developing evidence-based strategies that improve ACP uptake and ensure patients' end-of-life wishes are respected.
Barriers to Effective ACP Implementation
Several factors contribute to the underutilisation of ACP:
- Cultural and Emotional Challenges: Discussing end-of-life care is often considered taboo, leading to discomfort among patients and healthcare professionals. This discomfort can result in the avoidance of crucial conversations about future healthcare preferences (BMC Palliative Care, 2020).
- Lack of Education and Training: Healthcare professionals frequently report insufficient training in initiating ACP discussions. A study highlighted that the primary barriers to ACP include a lack of understanding and knowledge, as well as discomfort and resistance among healthcare providers (Journal of Hospice and Palliative Care, 2023).
- Time Constraints: The demanding nature of healthcare settings often leaves limited time for in-depth ACP discussions. This time pressure can prevent healthcare providers from engaging in meaningful conversations with patients about their end-of-life preferences (PubMed, 2019).
- Communication Gaps Among Services: Even when ACPs are in place, there is often a lack of effective communication between various healthcare providers, including general practitioners, community nurses, healthcare assistants, and emergency services. This disconnect can lead to situations where ACPs are not honoured due to unawareness among care teams.
Strategies for Enhancing ACP Engagement
Engagement with ACPs remains inconsistent, with many delaying discussions until a crisis arises. The North Cumbria End-of-Life Partnership (NCELP, 2024) highlights ACP as a priority, calling for a structured, proactive approach across Cumberland.
1. Public Education and Awareness
Raising awareness is crucial to normalising ACP discussions. Many people are unaware of its benefits or feel uncomfortable initiating conversations. The NCELP strategy highlights the need for targeted public education through community outreach, accessible materials, and engagement with underserved populations. Presenting ACP as a routine part of healthcare will encourage earlier decision-making.
2. Workforce Training
Healthcare professionals often lack confidence in discussing ACP. The NCELP strategy calls for structured training for GPs, nurses, and palliative care teams, ensuring they can guide patients sensitively and effectively. ACP education should be embedded into routine professional development, equipping all frontline staff with the necessary skills.
3. Embedding ACP into Healthcare Pathways
ACP must be integrated into routine care rather than treated as an isolated task. The NCELP strategy recommends incorporating ACP into long-term condition management, particularly for those with chronic illnesses or frailty. Using structured tools within primary care records will ensure ACP discussions are documented, updated, and revisited when necessary.
4. Improving Communication and Information Sharing
A major barrier to ACP is poor communication between services. The NCELP strategy highlights the need for shared digital records so that ACP decisions are accessible across GPs, hospitals, hospices, and care homes. Standardised protocols will ensure healthcare teams follow a consistent approach, reducing the risk of preferences being overlooked.
5. Strengthening Policy and Leadership
Embedding ACP into local commissioning plans is essential for long-term sustainability. The NCELP strategy calls for support from the ICB to prioritise ACP, secure funding for training and public awareness, and monitor uptake to address gaps. A coordinated approach will improve consistency across Cumberland’s health and care system.
By addressing these barriers and implementing targeted strategies, Cumberland can enhance the adoption and effectiveness of Advance Care Planning, ensuring that individuals' end-of-life preferences are respected and upheld.
Future Directions
End-of-life care in Cumberland needs to continue evolving towards a more community-based, person-centred approach, ensuring people can receive care where they feel most comfortable. Expanding hospice-at-home services and strengthening community palliative care will help reduce unnecessary hospital admissions and improve quality of life in the final stages. The North Cumbria End-of-Life Partnership (NCELP, 2024) is leading efforts to make this happen by focusing on workforce development, better coordination between services, and digital record-sharing to ensure seamless care.
A skilled and confident workforce is key to delivering high-quality palliative care. While there is a need for more specialist nurses and palliative care consultants, the NCELP strategy also highlights the importance of training GPs, community nurses, and social care workers, so they feel equipped to provide compassionate, end-of-life care. Advance Care Planning should become a routine part of healthcare, rather than something left until a crisis. Ensuring ACP discussions happen earlier, and that preferences are properly recorded and easily shared across healthcare services, will give people greater control over their final months.
Bereavement support also needs to be better integrated into palliative care, ensuring families and carers receive the emotional and practical help they need. Achieving all of this will require ongoing collaboration across health, social care, and voluntary sectors. By improving training, communication, and access to community-based care, Cumberland can help more people experience a dignified and well-supported end of life, in line with their wishes.
Chapter 8: A Call to Action – Preventing Ill Health and Improving Care Integration
Chapter 8: A Call to Action – Preventing Ill Health and Improving Care IntegrationAs Cumberland’s population continues to age, there is an urgent need to transition towards a preventative, integrated, and person-centred approach to health and social care. The rising prevalence of chronic conditions, frailty, and social determinants of health disparities demands proactive strategies that enable older adults to lead healthier, more independent lives. This chapter explores the key actions required to enhance health outcomes, alleviate pressure on healthcare services, and promote effective collaboration across various sectors.
Prioritising Prevention to Reduce Disease Burden
Prevention is central to reducing the long-term burden of disease among older adults. Research highlights that early interventions, lifestyle modifications, and community-led support significantly improve health outcomes (Public Health England, 2021). One critical component of this preventative approach is the early diagnosis and management of chronic diseases. Screening programmes for cardiovascular disease, diabetes, and dementia play a fundamental role in identifying conditions at an early stage, allowing for timely intervention and better management (NHS Digital, 2023). Additionally, encouraging participation in vaccination programmes—such as those for influenza, pneumococcal disease, and shingles—can help mitigate the risk of infectious diseases that disproportionately affect older adults (UK Health Security Agency, 2023).
A further pillar of prevention is the promotion of mobility and frailty reduction strategies. Physical activity remains one of the most effective ways to maintain strength and prevent falls, with initiatives such as Live Longer Better in Cumbria playing a pivotal role in promoting structured exercise for older residents (Active Cumbria, 2024). Falls prevention strategies, including home safety assessments and strength-based rehabilitation, are also vital in reducing hospital admissions related to fractures and mobility issues (British Geriatrics Society, 2023). Moreover, addressing malnutrition through community-based meal services and nutrition screening in primary care can have a profound impact on preventing frailty-related complications (Age UK, 2022).
Enhancing Mental Health and Social Wellbeing
The mental health of older adults is a crucial aspect of healthy ageing but often remains overshadowed by physical health concerns. Research demonstrates a strong link between social isolation and declining mental health, with loneliness being a significant contributor to depression and cognitive decline (Cumberland Council, 2023). Enhancing access to community-based mental health services, particularly in rural areas, is essential in providing older adults with support through talking therapies and social prescribing initiatives (NHS England, 2023).
Dementia-friendly community initiatives are increasingly recognised as an effective approach to supporting individuals with cognitive impairment and their carers, fostering an environment that encourages social engagement and reduces stigma (Alzheimer’s Society, 2023). Similarly, strengthening local networks for social inclusion—such as befriending services and intergenerational programmes—can play a crucial role in reducing feelings of isolation and improving overall wellbeing (Joseph Rowntree Foundation, 2023).
Addressing Health Inequalities and Social Determinants of Health
Older adults living in rural and socioeconomically deprived areas of Cumberland experience disproportionately poorer health outcomes due to barriers in accessing essential healthcare services, transport, and social support. Addressing these health inequalities requires targeted investment in infrastructure and services to ensure equitable access to healthcare and community resources. Improving rural transport networks can significantly enhance healthcare accessibility, particularly for older adults who rely on public transport to attend medical appointments (Cumbria County Council, 2023).
Additionally, housing conditions play a critical role in supporting ageing in place. Increasing financial assistance for home adaptations, such as grab rails, stairlifts, and accessible bathrooms, can enable older individuals to continue living safely and independently in their homes (Cumberland Housing Group, 2023). Furthermore, expanding digital health literacy programmes is vital to ensuring that older residents can confidently navigate online healthcare services and telemedicine options, thereby reducing disparities in access to healthcare information and support (Public Health England, 2021).
Strengthening Integrated Care and Workforce Capacity
Given the complexity of older adults’ healthcare needs, a coordinated and integrated approach is imperative. The Proactive Care Pilot Programme in Cumberland has demonstrated the benefits of a multidisciplinary model in reducing hospital admissions and enhancing continuity of care (Year of Care Partnerships, 2024). Building upon this, expanding Integrated Care Hubs that bring together healthcare, social care, and voluntary sector services can further improve patient outcomes by providing a holistic, person-centred approach to care. Strengthening collaboration between primary care, community health teams, and adult social care services will also be essential in streamlining patient pathways and minimising the risk of unnecessary hospitalisation (Health Foundation, 2023).
Workforce training and retention are equally critical in sustaining high-quality care provision for older adults. Investing in specialised training programmes for frailty management and end-of-life care can equip healthcare professionals with the necessary skills to address the complex needs of the ageing population (Kings Fund, 2023). Retaining and recruiting care workers, particularly in rural areas, will require financial incentives, career development opportunities, and improved working conditions to ensure a stable and well-supported workforce (Health Education England, 2023). Moreover, expanding the role of community health workers and social prescribers will strengthen the support network available to older adults, empowering them to manage their health conditions more effectively (British Geriatrics Society, 2023).
The Path Forward: A Collaborative Commitment
Ensuring that Cumberland’s ageing population can lead healthy, independent, and dignified lives will require a concerted effort from multiple stakeholders. Strong leadership, policy alignment, and community engagement are key to fostering an age-friendly society. Strategic investment in preventative care, integrated service models, and workforce development must be prioritised to create a sustainable and resilient health and social care system. Aligning local policies with national frameworks, such as the NHS Long Term Plan and Ambitions for Palliative and End-of-Life Care, will also provide a structured approach to improving services for older residents.
Furthermore, robust monitoring and evaluation mechanisms must be established to track progress, assess the impact of interventions, and adapt strategies based on emerging evidence. By embracing these approaches, Cumberland can set a precedent in promoting healthy ageing, ensuring that older adults not only live longer but also enjoy an improved quality of life, autonomy, and overall wellbeing.
Recommendations and Conclusions
As Cumberland’s population continues to age, ensuring that older adults can live well, stay independent, and access high-quality care is more important than ever. This report has explored the key challenges they face—from social isolation and healthcare access to housing, digital literacy, frailty, and end-of-life care. While progress has been made, particularly in areas like community palliative care and frailty management, many older residents still struggle to get the support they need, especially in rural and disadvantaged areas.
To meet these challenges, Cumberland must take a coordinated, person-centred approach, where health, social care, and community services work seamlessly together. Building an Age-Friendly Cumberland (Chapter 2) provides the foundation for this vision, aligning with the WHO Age-Friendly Cities framework, which promotes inclusive communities, accessible services, and integrated healthcare. By embedding these principles into local policies and services, Cumberland can create a system where older residents not only receive the care they need but also feel valued and connected to their communities.
Moving forward, the focus must be on practical, impactful changes. The following recommendations set out the strategic priorities that will guide Cumberland’s approach to ageing well, ensuring that services evolve to meet the needs of its growing older population.
Key Recommendations
1. Strengthening Social Inclusion and Community Support
- Expand rural transport services to improve mobility and reduce social isolation, particularly for those in remote areas.
- Increase funding for community-based activities, including intergenerational programmes, age-friendly community hubs, and social clubs.
- Promote age-inclusive policies in businesses and public services to support participation in economic and social life.
2. Improving Access to Healthcare and Preventative Care
- Expand frailty screening and early intervention programmes to prevent deterioration and hospital admissions.
- Strengthen integration between health and social care services to improve coordination, reduce delays, and provide seamless care transitions.
- Improve access to mental health services, including dementia support and depression screening, particularly for isolated older adults.
3. Enhancing Housing and Accessibility
- Increase the availability of affordable, age-friendly housing, ensuring new developments meet accessibility needs.
- Expand home adaptation grants to support older adults in making necessary modifications to their homes.
- Improve integration between housing, health, and social care services, enabling more people to remain independent at home.
4. Bridging the Digital Divide
Expand digital literacy programmes to equip older adults with the skills to access and navigate online healthcare, while ensuring ongoing, guided support rather than one-off training sessions.
Improve broadband connectivity in rural areas, while ensuring affordable access schemes are in place for older residents who may struggle with the costs of digital services.
Develop accessible and age-friendly digital health platforms, ensuring that online NHS services and local public services are clear, user-friendly, and designed with older adults in mind.
Maintain a hybrid approach to healthcare access, ensuring that face-to-face and telephone options remain available alongside digital services, preventing digital exclusion.
Increase trust in digital health tools, such as the NHS App, by improving user support, addressing security concerns, and promoting community-led peer learning initiatives.
5. Strengthening Proactive Frailty Management
- Scale up the Proactive Care Pilot Programme, supporting early identification of frailty and preventative interventions.
- Increase workforce training for primary care staff and community health teams in frailty care and prevention.
- Expand falls prevention initiatives, ensuring strength and balance programmes are widely accessible.
6. Enhancing End-of-Life Care and Advance Care Planning
Expand home-based palliative care services to reduce unnecessary hospital admissions and ensure more people receive care in their preferred setting.
Embed ACP into routine healthcare interactions, ensuring that discussions happen earlier and are properly documented.
Strengthen training for healthcare professionals, including GPs, community nurses, and social care workers, so they feel confident initiating ACP discussions.
Improve digital integration of ACP records, allowing preferences to be easily accessed and honoured across primary care, hospitals, and hospices.
Ensure clearer pathways for enacting ACP decisions, so that individuals with active care plans have their wishes respected without unnecessary delays.
7. Addressing Health Inequalities and Workforce Challenges
- Prioritise investment in rural and disadvantaged areas, ensuring equitable access to healthcare, housing, and social care.
- Strengthen workforce recruitment and retention, particularly in palliative care, frailty management, and community nursing.
- Expand public awareness campaigns around ageing, dementia, and ACP to promote informed decision-making and reduce stigma.
Moving Forward
By implementing these strategic recommendations, Cumberland can create a more inclusive, supportive, and sustainable system of care for its ageing population. The success of these initiatives will depend on continued collaboration between local authorities, healthcare providers, voluntary organisations, and the broader community.
While progress has been made in key areas, including frailty prevention, proactive care, and palliative care expansion, further efforts are needed to address workforce shortages, reduce health inequalities, and integrate services more effectively.
A future where older adults in Cumberland can live, age, and die well is within reach, as long as we remain committed to evidence-based policies, community-driven initiatives, and long-term investment in health and social care infrastructure.
Acknowledgements
AcknowledgementsI would like to thank all those who have contributed to the preparation of this Public Health Annual Report, including:
- Claire King, Public Health Consultant
- Joanna Coleman, Public Health Manager
- Clare Paling, Development Officer, Active Cumbria
- Ed Tallis, ICB Director of Delivery – North Cumbria
- Laura Marshall, Commissioning Manager – North Cumbria Local Delivery Team
- Debbie McKenna, CEO, Hospice at Home Carlisle and North Lakeland
- Julie Clayton, Chief Executive, Eden Valley Hospice
- Robert Westgate
- Clare Edwards, Health Partnership Manager
I also thank the wider public health and adult social care teams at Cumberland Council, along with community partners, clinicians, and members of the Age-Friendly Board and NCELP, whose input has shaped this report. I am especially grateful to the data and intelligence teams for their support. Most importantly, I acknowledge the older residents of Cumberland, whose lived experiences, resilience, and continued contributions to our communities remain at the heart of this report and its vision for healthy ageing.
And finally, particular thanks to Faisal Solkar, our Public Health Specialist Registrar, who co-ordinated everyone’s input and acted as lead author for this report.
Bibliography
BibliographyActive Cumbria (2024) Live Longer Better in Cumbria: Activity Guides for Older Adults. Available at: https://www.activecumbria.org.
Age UK (2022) Later Life in the United Kingdom. Available at: https://www.ageuk.org.uk.
Age UK Carlisle & Eden (2022) Age-Friendly Community Research Final Report. Carlisle: Age UK Carlisle & Eden.
Alzheimer’s Society (2023) Dementia Statistics Hub. Available at: https://www.alzheimers.org.uk.
BMC Palliative Care (2020). Barriers to advance care planning: a qualitative study of seriously ill patients' perspectives. Available at: https://bmcpalliatcare.biomedcentral.com/articles/10.1186/s12904-020-00587-0
British Geriatrics Society (2023) Frailty: A Key Priority for Care. Available at: https://www.bgs.org.uk.
British Medical Journal (2013). Only 5% of British people have made advance care plans, survey finds. Available at: https://www.bmj.com/content/346/bmj.f3073
Carlisle Healthcare (2024) Elderly Care Services. Available at: https://www.carlislehealthcare.co.uk.
Care Quality Commission (2022) Care Homes in Cumberland. Available at: www.cqc.org.uk.
Cumbria County Council (2023) Transport and Access in Rural Areas. Available at: https://www.cumbria.gov.uk.
Cumbria Housing Group (2023) Housing Needs of the Elderly. Available at: https://www.cumbriahousing.org.uk.
Cumbria Observatory (2023) Population Trends in Cumberland. Available at: https://www.cumbriaobservatory.org.uk.
Cumberland Council (2023) Digital Inclusion Strategy for Cumberland. Available at: www.cumberland.gov.uk.
Cumberland Council (2023) Extra Care Housing Strategy. Available at: www.cumberland.gov.uk.
Cumberland Council. (2023). Housing for Older People in Allerdale. Available at: https://www.allerdale.gov.uk/en/housing/find-home/housing-older-people-allerdale
Cumberland Council (2023) Market Position Statement for Adult Social Care Services 2025-2029. Available at: www.cumberland.gov.uk.
Cumberland Council (2024) Market Position Statement for Adult Social Care Services 2025-2029. Available at: https://www.cumberland.gov.uk.
Department of Health and Social Care (2023) Chief Medical Officer’s Annual Report 2023: Health in an Ageing Society. Available at: https://assets.publishing.service.gov.uk/media/6674096b64e554df3bd0dbc6/chief-medical-officers-annual-report-2023-web-accessible.pdf
Eden Country Care (2024) Elderly Social Care Services. Available at: https://www.edencountrycare.co.uk.
Eden Valley Hospice (2024) Palliative Care Services. Available at: https://www.edenvalleyhospice.org.
Greenhalgh, T., Wherton, J., Shaw, S., & Morrison, C. (2023). Digital health inequalities: Why the digital-first NHS may exacerbate disparities in care. Journal of Medical Internet Research, 25, e45672.
Grüning, L., Cahill, R., and Latif, S. (2023) Determinants of digital health literacy in older populations: A systematic review. Frontiers in Public Health, 11, 1447747. Available at: https://www.frontiersin.org.
Health Education England (2023) Workforce Development for an Ageing Population. Available at: https://www.hee.nhs.uk.
Health Foundation (2023) Proactive Care Models: Reducing Pressure on Acute Services. Available at: https://www.health.org.uk.
Journal of Hospice and Palliative Care (2023). Barriers to Effective Communication about Advance Care Planning. Available at: https://www.e-jhpc.org/journal/view.html?uid=516&vmd=Full
Joseph Rowntree Foundation (2023) Poverty in the UK. Available at: https://www.jrf.org.uk.
Kings Fund (2023) Meeting the Health and Care Needs of an Ageing Population. Available at: https://www.kingsfund.org.uk.
Macmillan Cancer Support (2017). Missed Opportunities: Advance Care Planning Report. Available at: https://www.macmillan.org.uk/_images/missed-opportunities-end-of-life-advance-care-planning_tcm9-326204.pdf
NHS Digital (2023) Health Conditions Statistics. Available at: https://digital.nhs.uk.
NHS England (2021) Ambitions for Palliative and End of Life Care: A national framework for local action 2021-2026. Available at: https://www.england.nhs.uk.
NHS England (2023) Integrated Digital Health Solutions for Primary Care. Available at: https://www.england.nhs.uk.
NICE (2015) Care of dying adults in the last days of life [NG31]. Available at: https://www.nice.org.uk.
NICE (2023) Falls Prevention in Older Adults: Guidelines and Recommendations. Available at: https://www.nice.org.uk.
NICE (2023) Managing Polypharmacy in Older Adults. Available at: https://www.nice.org.uk.
North Cumbria End-of-Life Partnership (NCELP) (2024) End-of-Life Care Strategy and Delivery Plan: Priorities for North Cumbria.
North Cumbria Integrated Care NHS Foundation Trust, 2025. Information Governance
North Cumbria Integrated Care NHS Foundation Trust (2025) Palliative Care Services. Available at: https://www.ncic.nhs.uk.
North Cumbria Place-Based Partnership (2025). Frailty Strategy for North Cumbria 2025-2029. North Cumbria Integrated Care Partnership.
Office for National Statistics (ONS) (2023) Population Estimates for the UK. Available at: https://www.ons.gov.uk.
Office for National Statistics (ONS) (2023) Winter mortality in England and Wales - Office for National Statistics
Palmer, K. T., Craven, M. P., & Barker, R. O. (2023). Barriers to NHS App uptake among older adults: A mixed-methods study on digital exclusion in primary care. BMJ Open, 13(4), e064912.
Public Health England (2020) Tackling Loneliness: A Public Health Approach.
Public Health England (2021) Health Inequalities and Digital Inclusion. Available at: https://www.gov.uk/government/organisations/public-health-england.
Public Health England (2021) Health and Housing: Evidence Review.
Public Health England (2023) Health Inequalities and Digital Inclusion. Available at: https://www.gov.uk/government/organisations/public-health-england.
Public Health England (2023) Health Inequalities in Rural Communities. Available at: https://www.gov.uk/government/organisations/public-health-england.
Public Health England (2023) Palliative and End of Life Care Profiles: December 2023 Update. Available at: https://www.gov.uk/government/statistics.
PubMed (2019). Barriers to advance care planning with patients as perceived by nurses and other healthcare professionals: a systematic review. Available at: https://pubmed.ncbi.nlm.nih.gov/31494997/
Robinson, L., Dickinson, C., Bamford, C., et al. (2022). Advance care plans in UK care home residents: a service evaluation of interventions in a primary care setting. Age and Ageing, 51(3), afac069. Available at: https://academic.oup.com/ageing/article/51/3/afac069/6555262
Watson, N., Protheroe, J., & Steel, N. (2022). Digital health literacy and older adults: The role of guided support and social learning in technology adoption. Ageing & Society, 42(6), 1254–1273.
World Health Organization (WHO) (2007) Global age-friendly cities: A guide. Available at: https://iris.who.int/bitstream/handle/10665/43755/9789241547307_eng.pdf
Year of Care Partnerships (2024) Proactive Care Pilot Programme Report. Available at: https://www.yearofcare.co.uk.
Zhao, Y., Zhang, H., and Li, X. (2022) The impact of digital health literacy interventions on health outcomes among older adults: A meta-analysis. Journal of Medical Internet Research, 24(6), e10365623. Available at: https://www.jmir.org.