Chapter 1: The Ageing Population of Cumberland - Demographics and Health Insights
Chapter 1: The Ageing Population of Cumberland - Demographics and Health InsightsThe elderly population in Cumberland represents a significant and growing proportion of the community, bringing unique challenges and opportunities for health and social care services. Understanding the demographic characteristics and social determinants affecting older adults is essential for designing effective interventions and policies.
Current Demographic Data
Population Size
Cumberland’s population aged 65 and over has seen consistent growth in recent years, reflecting national trends of an ageing population. The 2021 Census data highlights that Cumberland has a significantly older population compared to both the Northwest region and England as a whole. As shown in Table 1, 23.2% of Cumberland’s population is aged 65 and over, exceeding the Northwest (18.7%) and England (18.4%) averages. This demographic trend indicates a clear shift towards an ageing population, with an increasing proportion of older residents compared to regional and national figures (ONS, 2023).
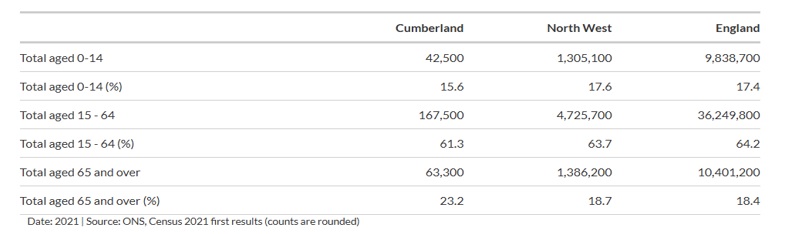
Table 1: Age Distribution in Cumberland, Northwest, and England
Source: ONS, Census 2021
Further demonstrating this trend, Figure 1 presents the population distribution by five-year age groups, comparing Cumberland with England. The graph shows that Cumberland has a noticeably larger proportion of older adults, particularly in the 65+ and 85+ age brackets, than the national average. The proportion of people aged 85 and over is projected to grow by over 30% in the next decade, highlighting a continuing demographic shift (Age UK, 2022).
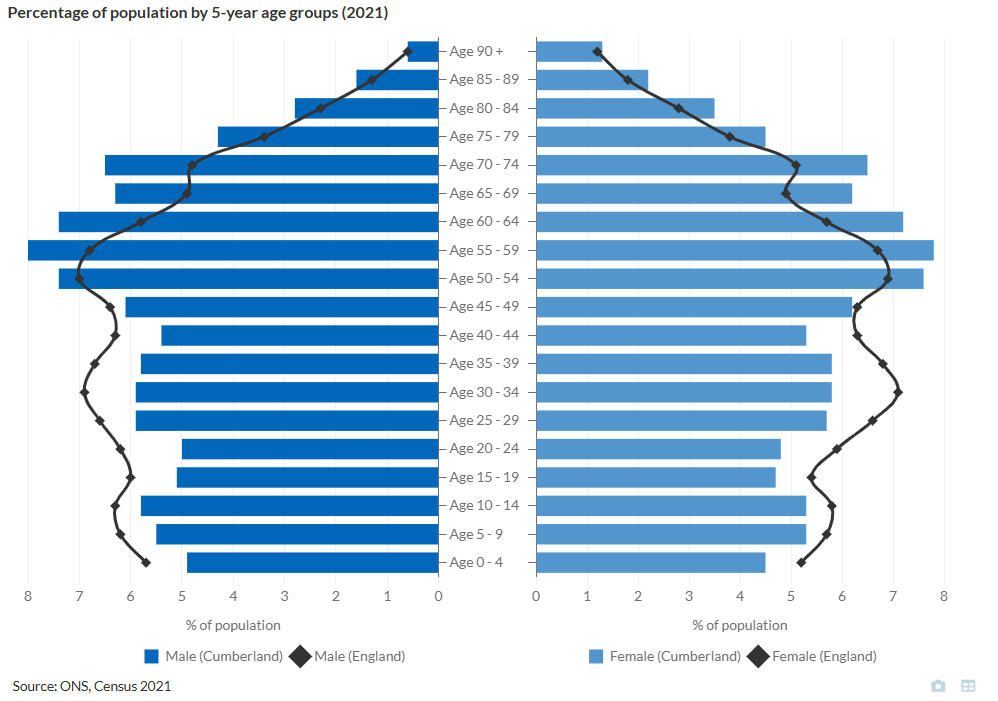
Figure 1: Population Distribution by 5-Year Age Groups in Cumberland and England
Source: ONS, Census 2021.
Geographical Distribution
Using the 2021 census data, we can breakdown Cumberland into districts and can see variation in the age distribution of people 65 and over in Cumberland.
| Area | Population 65+ (%) |
|---|---|
| Allerdale | 25 |
| Carlisle | 20 |
| Copeland | 21 |
Table 2: Population Aged 65 and Over by Area in Cumberland (2021 Census)
Source: ONS, Census 2021
Allerdale and Copeland are more rural than Carlisle, which has large rural areas but also a key urban centre that contains around half of its population. The higher percentage of older adults in Allerdale (25%) reflects a common trend observed in rural areas, where populations tend to age more rapidly. This is often due to younger people migrating towards urban centres like Carlisle in search of employment, education, and better access to services, leaving behind an older demographic in more remote locations.
Rurality presents unique public health challenges for these areas. Older adults in rural communities often face difficulties accessing primary care, specialist services, and emergency healthcare due to longer travel distances and fewer local facilities. Additionally, the lack of transport links and limited opportunities for social engagement can increase the risk of social isolation and loneliness, further impacting mental health and well-being.
Life Expectancy
Life expectancy in Cumberland is 79 years for men and 83 years for women, slightly below the national averages of 80 years for men and 84 years for women (Public Health England, 2023). However, these figures mask significant disparities in both total life expectancy and healthy life expectancy, particularly between rural and socioeconomically deprived areas.
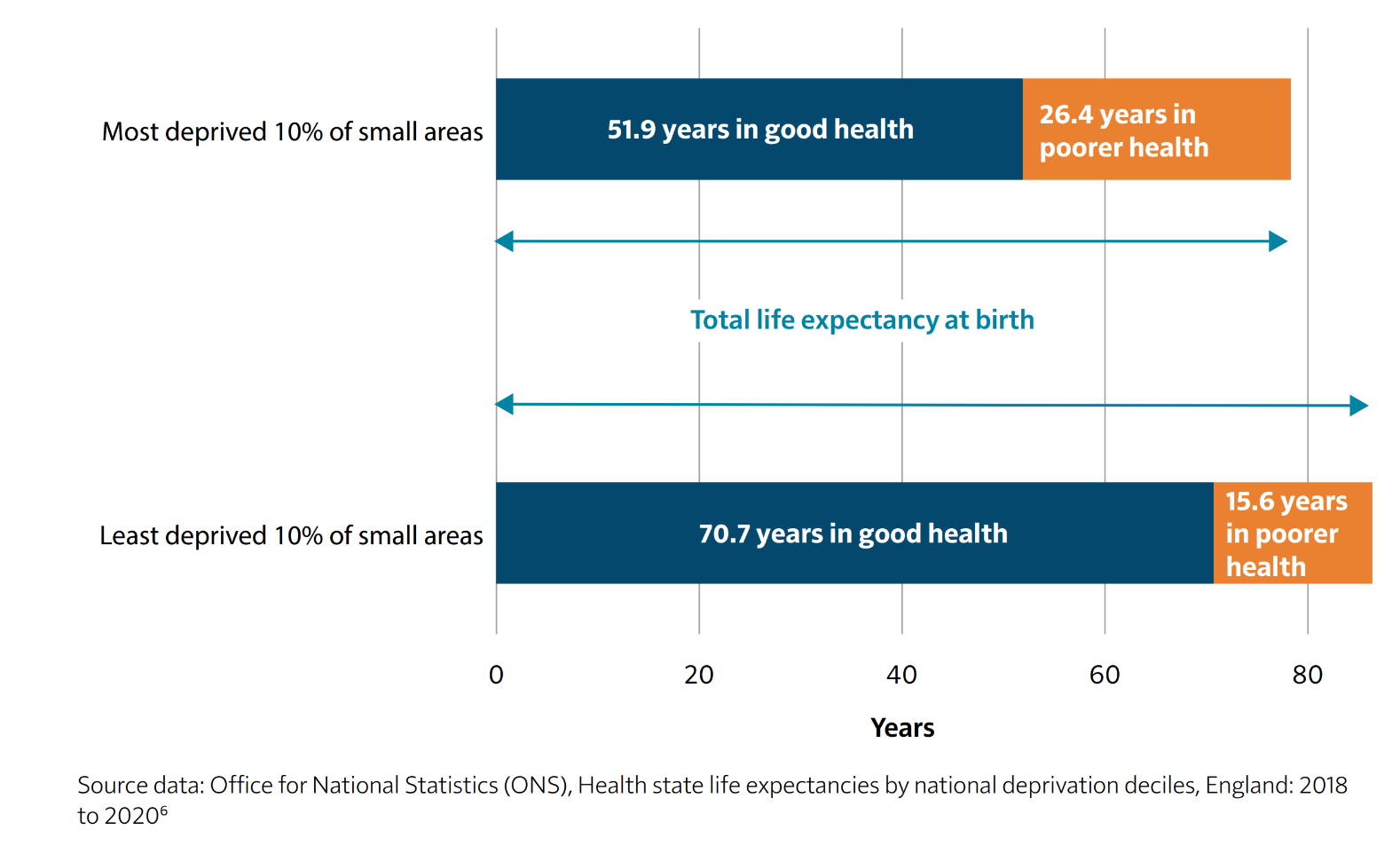
Figure 2: Life Expectancy and Healthy Life Expectancy by Deprivation Level in England (2018–2020)
Source: Office for National Statistics (ONS), Health State Life Expectancies by National Deprivation Deciles, England: 2018 to 2020.
As illustrated in Figure 2, individuals in the most deprived areas not only have shorter life expectancies but also spend a significantly larger proportion of their later years in poor health. In Cumberland’s more deprived communities, older adults face higher rates of long-term illness, poorer access to healthcare, and greater levels of social isolation, all of which contribute to a shorter life expectancy and lower quality of life in later years. The graph highlights that those in the most deprived areas spend an average of 26.4 years in poor health, compared to just 15.6 years in the least deprived areas, reflecting stark inequalities in healthy ageing.
Conversely, older adults in more affluent or rural parts of Cumberland tend to live longer and in better health, often benefiting from lower pollution levels, stronger social networks, and healthier lifestyles. However, even in these areas, challenges remain, particularly concerning access to healthcare services, availability of social care, and transportation barriers, all of which are crucial for supporting independent living among the elderly.
Healthy Life expectancy
Healthy life expectancy (HLE) is a crucial indicator of population health, representing the number of years an individual can expect to live in good health. It reflects not just longevity but also the quality of life and the effectiveness of local health and social care systems. In Cumberland, HLE trends suggest key challenges and disparities when compared to neighbouring areas such as Westmorland & Furness, wider Cumbria, and national averages.
Trends in Healthy Life Expectancy
Between 2012 and 2022, Cumberland has experienced a decline in HLE for both males and females. In 2012, male HLE at birth in Cumberland stood at 61.4 years, peaking at 62.81 years in 2016, before steadily declining to 58.38 years by 2022. Similarly, female HLE at birth started at 62.1 years in 2012, peaked at 63.96 years in 2016, and dropped to 59.13 years in 2022. This decline suggests increasing health inequalities and potential concerns regarding the effectiveness of preventive health measures and social care provision.
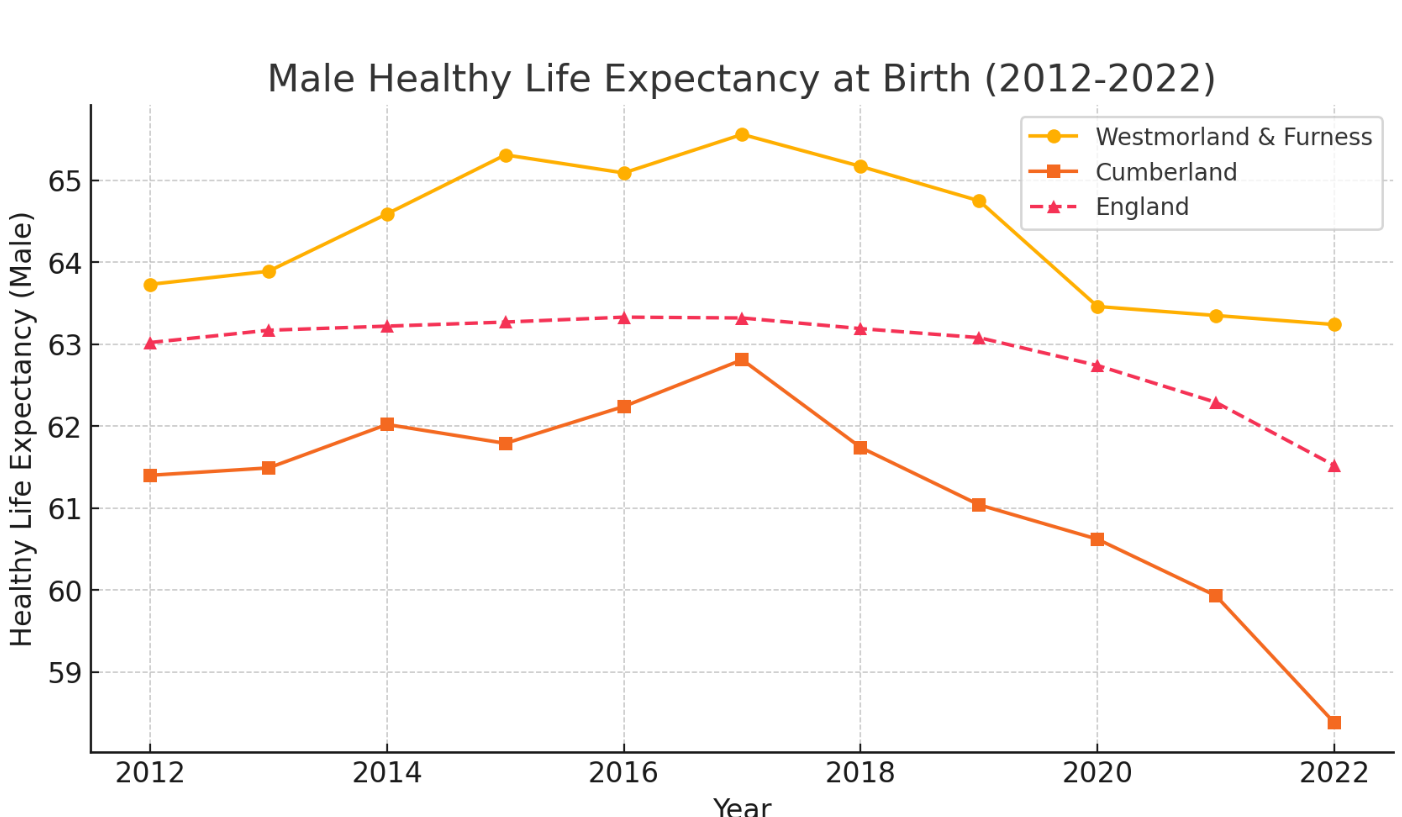
Figure 3: Male Healthy Life Expectancy at Birth in Cumberland, Westmorland & Furness, and England (2012–2022)
Source: Office for National Statistics (ONS), 2023.
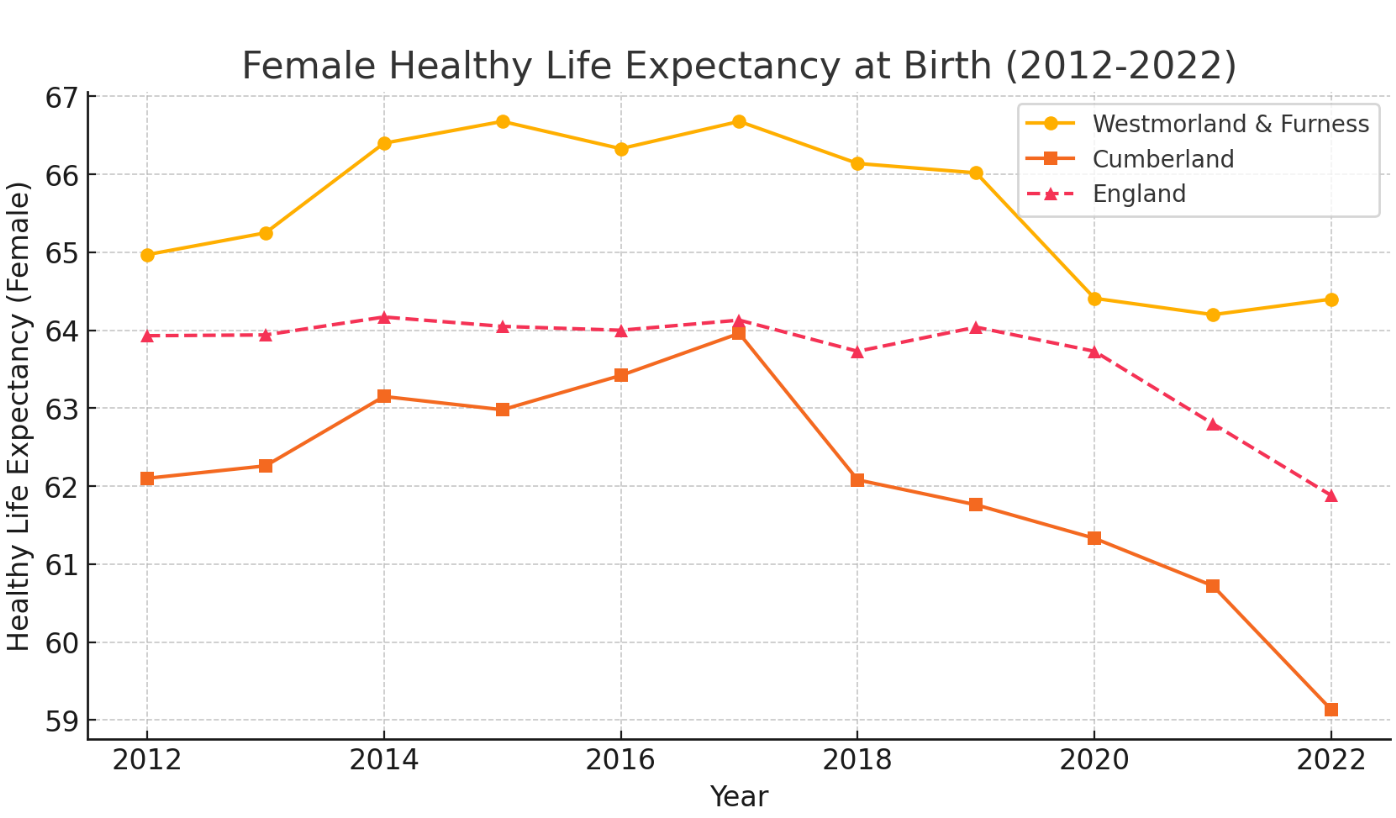
Figure 4: Female Healthy Life Expectancy at Birth in Cumberland, Westmorland & Furness, and England (2012–2022)
Source: Office for National Statistics (ONS), 2023.
In contrast, Westmorland & Furness has consistently demonstrated a higher HLE across the decade, because people in this area, on average, have higher incomes and better living conditions. Male HLE in 2012 was 63.73 years, rising to 65.56 years in 2017, before experiencing a slight decline to 63.24 years in 2022. Female HLE followed a similar trajectory, peaking at 66.68 years in 2014 and 2017, before decreasing to 64.4 years in 2022.
The higher HLE in Westmorland & Furness is strongly linked to socioeconomic advantages, as the region remains on average more affluent than Cumberland despite having some significant pockets of deprivation.
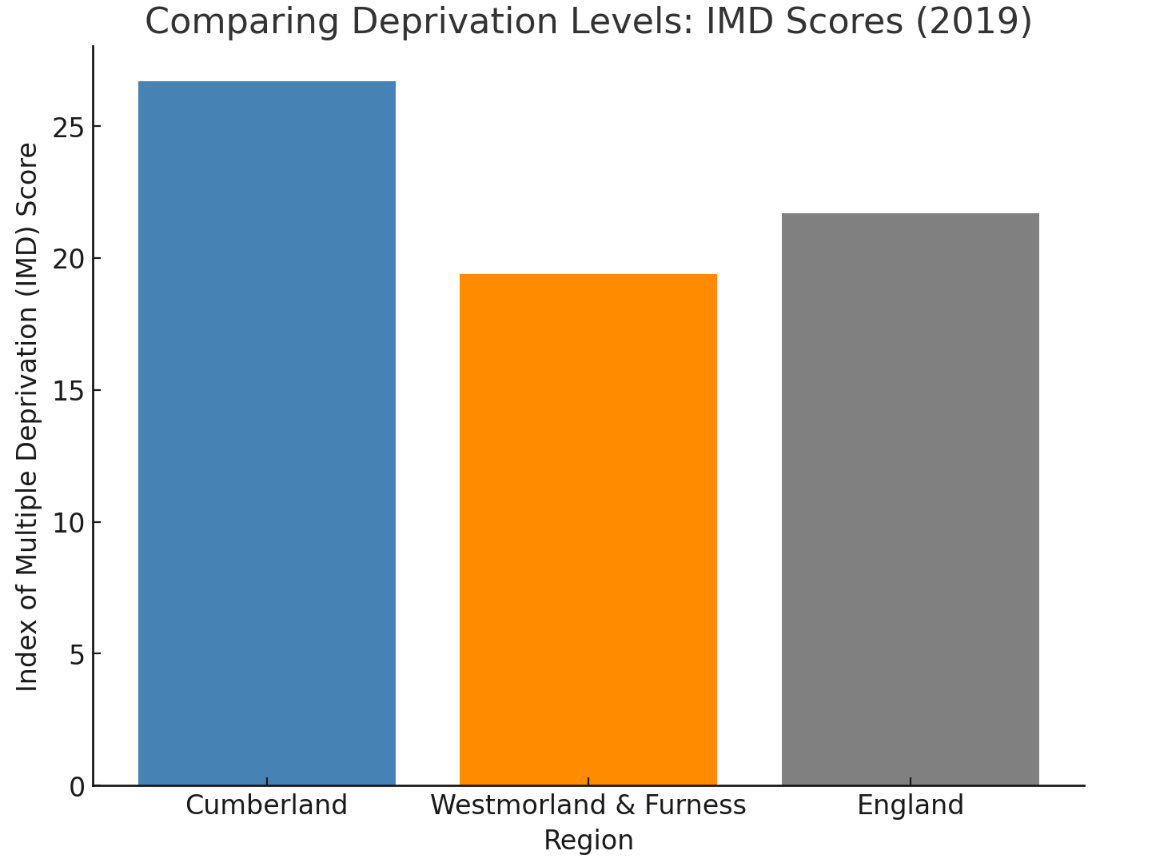
Figure 5: Comparing Deprivation Levels – Index of Multiple Deprivation (IMD) Scores (2019)
Source: English Indices of Deprivation, Ministry of Housing, Communities & Local Government (2019).
Higher income levels, better housing conditions, and increased access to preventive healthcare services contribute to healthier ageing outcomes (ONS, 2023; Public Health England, 2023). Socioeconomic disparities impact lifestyle choices, including diet, physical activity, and smoking prevalence, all of which are major determinants of HLE (The King’s Fund, 2023). In contrast, Cumberland has a higher proportion of deprived communities, which correlates with greater levels of long-term illness and earlier onset of frailty (Joseph Rowntree Foundation, 2023).
At the national level, England’s male HLE was 63.02 years in 2012, showing a gradual decline to 61.52 years by 2022, a trend mirrored in female HLE. This indicates a broader national issue of declining healthy years lived, potentially linked to factors such as an ageing population, increasing levels of chronic diseases, and the long-term impacts of economic and health inequalities.
Regional Disparities and Key Considerations
Comparing Cumberland’s figures to the wider Cumbria region, a similar pattern emerges, with the county's HLE being higher in more affluent and rural areas like Westmorland & Furness but declining in areas with higher levels of deprivation, including parts of Cumberland. This highlights persistent health inequalities within Cumbria, where variations in access to healthcare, employment opportunities, and social support networks play a significant role in determining health outcomes.
Excess Winter Deaths in Cumberland
Winter brings with it an increased risk of illness and mortality, particularly for older adults. Cold temperatures, seasonal infections, and fuel poverty contribute to excess winter deaths (EWD), which refer to the additional deaths occurring in the winter months compared to the rest of the year. Data from the Office for National Statistics (ONS) for 2020/21, which includes COVID-19-related deaths, reveals stark regional disparities.
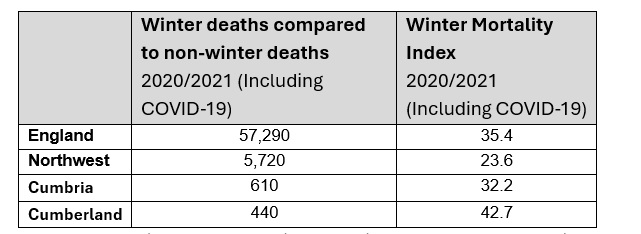
Table 3: Excess Winter Deaths and Winter Mortality Index (2020/2021, Including COVID-19)
Source: Office for National Statistics (ONS), 2021
Cumberland recorded 440 excess winter deaths, with a Winter Mortality Index (WMI) of 42.7 - the highest among the areas analysed. The WMI measures the percentage increase in deaths during the winter months (December to March) compared to the non-winter months, offering an indication of how significantly winter impacts mortality. A higher WMI suggests a greater seasonal effect on deaths. Cumberland’s WMI of 42.7 highlights that winter mortality in the area was disproportionately high compared to both the Northwest (23.6 WMI) and the national average (35.4 WMI). Cumbria as a whole also reported a higher-than-average WMI of 32.2, reinforcing the particular challenges faced by rural communities.
Several factors contribute to these figures. Older people are particularly vulnerable, with pre-existing conditions such as cardiovascular disease, respiratory illnesses, and frailty exacerbating the effects of cold weather. Housing conditions play a crucial role, as many older residents in Cumberland live in poorly insulated homes that are expensive to heat, increasing the likelihood of cold-related illnesses. The region’s rural geography also presents a challenge, with limited access to healthcare services making it harder to receive timely treatment during winter months.
The impact of COVID-19 cannot be overlooked. The pandemic placed additional strain on health services, while restrictions on social contact may have reduced the ability of families and carers to support elderly relatives, leading to delayed medical attention for winter-related illnesses.
Reducing Winter Mortality in Cumberland
A comprehensive approach is needed to tackle excess winter deaths in Cumberland, focusing on housing conditions and healthcare access. Cold homes significantly increase the risk of respiratory and cardiovascular illnesses, particularly in rural areas where older housing and off-grid energy make heating costly. To address this, affordable warmth initiatives should prioritise home insulation schemes, financial support for heating costs, and cold weather action plans providing fuel vouchers and emergency heating assistance.
Alongside housing improvements, better healthcare outreach is vital to prevent winter illnesses. Influenza and pneumonia remain leading causes of seasonal deaths, particularly for older adults with chronic conditions. However, vaccine uptake is lower in rural areas due to transport barriers and limited access to healthcare. Expanding mobile vaccination clinics, home visits, and targeted promotion through GP practices and pharmacies would help protect those most at risk. Strengthening partnerships between primary care, local councils, and community organisations can further improve vaccine access and winter health support. By tackling fuel poverty and healthcare access, Cumberland can reduce preventable winter deaths and improve outcomes for its ageing population.
Winter deaths are largely preventable, and targeted interventions could help reduce the seasonal strain on health and social care services. Ensuring that older adults in Cumberland remain warm, well-supported, and connected to healthcare in colder months is a public health priority.
The Burden of Disease and Chronic Conditions
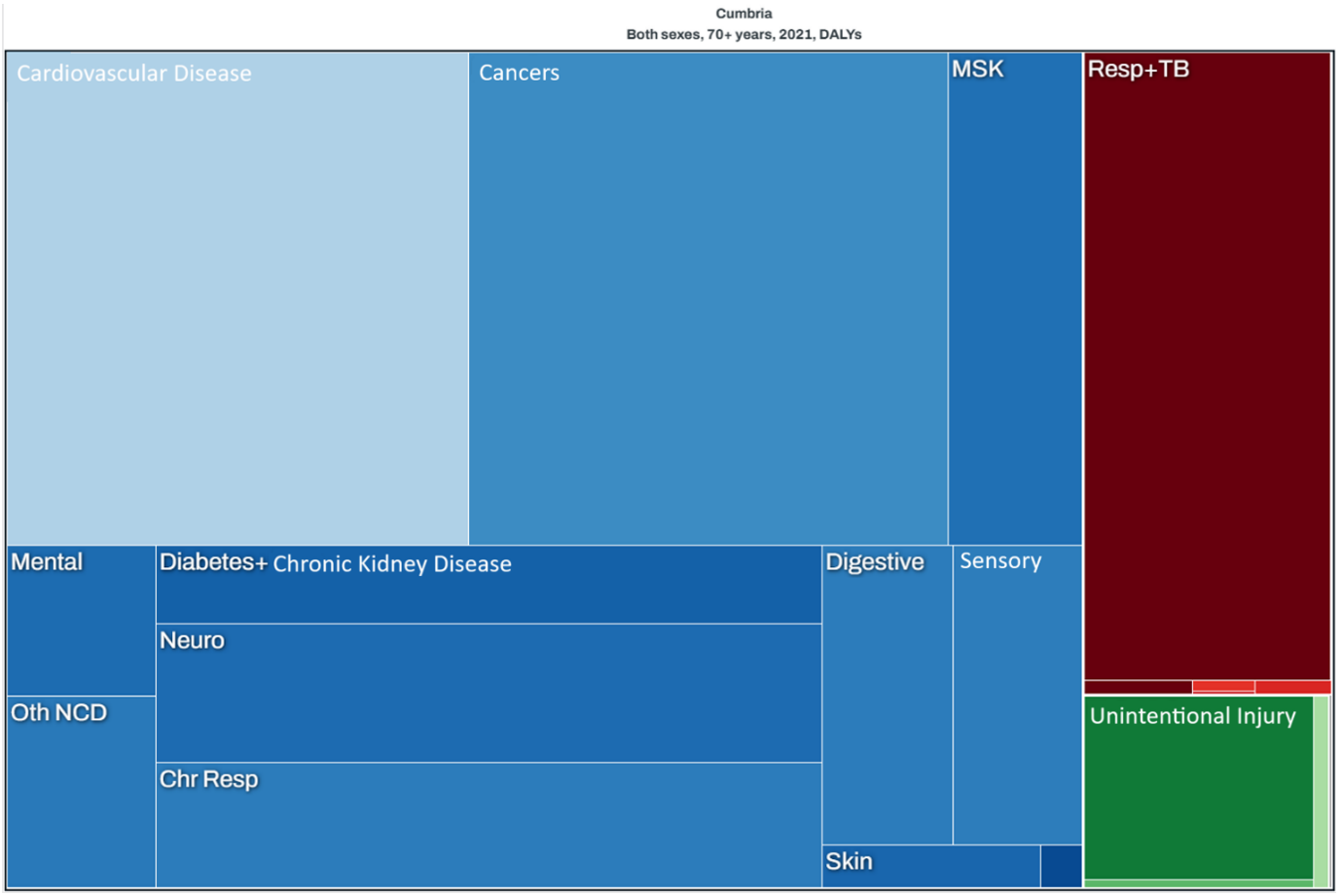
Figure 6: Burden of Disease in Cumbria (Both Sexes, 70+ Years, 2021) – Disability-Adjusted Life Years (DALYs)
Source: Global Burden of Disease Study, Institute for Health Metrics and Evaluation (IHME), 2021
The tree map, illustrates the major health conditions affecting adults aged 70 and over in Cumbria, measured in Disability-Adjusted Life Years (DALYs), a metric that captures both premature mortality and years lived with disability. Larger rectangles indicate a greater disease burden, with different colours representing distinct categories of illness.
Cardiovascular diseases, particularly heart disease and strokes, account for the greatest proportion of health loss in older adults, followed closely by cancers. Lung diseases, including chronic obstructive pulmonary disease (COPD) and respiratory infections, are also significant contributors. Musculoskeletal conditions such as arthritis and osteoporosis impact mobility and independence, while diabetes, kidney disease, dementia, and mental health disorders contribute to long-term disability. Hearing and vision impairment, digestive issues, and chronic lung diseases are present but have a smaller impact.
Falls and injuries remain a concern, particularly in those with frailty, though their contribution to overall disease burden is lower than that of chronic illnesses. These patterns highlight the importance of preventative care, mobility support, and fall prevention strategies to promote independence and reduce hospital admissions.
Chronic Diseases and Multimorbidity
Older adults in Cumberland commonly experience a range of chronic health conditions, which often co-exist, leading to multimorbidity and more complex healthcare needs.
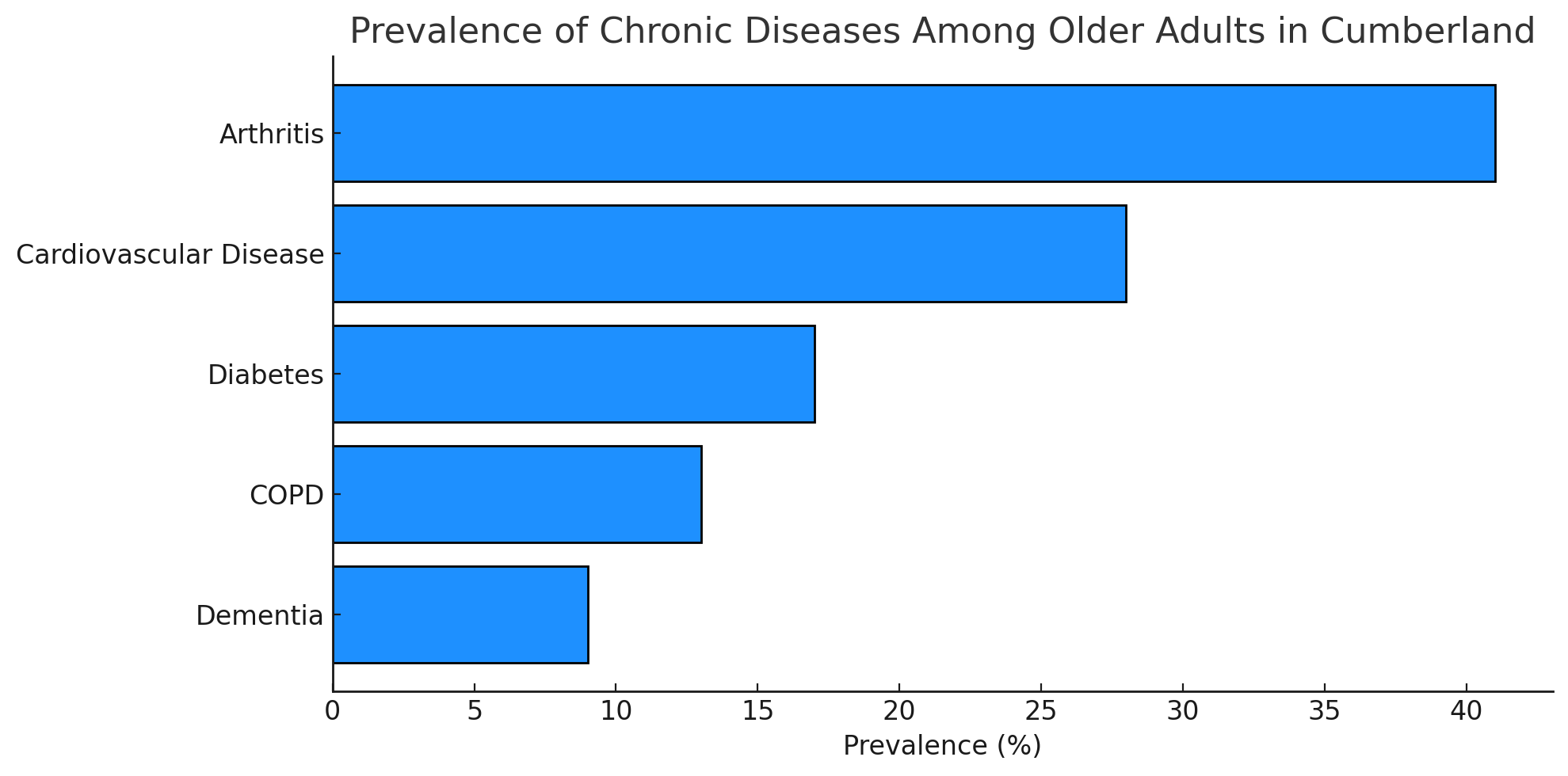
Figure 7: Prevalence of Chronic Diseases Among Older Adults in Cumberland (2023)
Source: Compiled from NHS Digital, British Geriatrics Society, and Alzheimer's Society, 2023.
The most prevalent conditions include:
- Cardiovascular Disease (CVD): Approximately 28% of older adults in Cumberland are affected, with high rates of hypertension and heart disease (NHS Digital, 2023).
- Diabetes: Affecting around 18% of those aged 65 and over, diabetes significantly increases the risk of complications such as neuropathy and kidney disease (NHS Digital, 2023).
- Chronic Obstructive Pulmonary Disease (COPD): With a 12% prevalence, COPD is a leading cause of hospitalisation in older adults.
- Arthritis and Musculoskeletal Conditions: Over 40% of older adults report joint pain or mobility issues due to osteoarthritis and rheumatoid arthritis (British Geriatrics Society, 2023).
- Dementia: Approximately 9% of Cumberland’s older population has dementia, with a projected 25% increase in cases by 2035 (Alzheimer’s Society, 2023).
Frailty and Its Impact on Healthcare Demand
Frailty is a major concern among Cumberland’s older adults, particularly those over 80, leading to increased hospital admissions, care dependency, and loss of independence. Defined as a condition where minor health issues can trigger severe declines in health, frailty is becoming more prevalent as the population ages (British Geriatrics Society, 2023).
Physical inactivity accelerates muscle loss, increasing the risk of falls and fractures. Many older adults also experience polypharmacy, where taking multiple medications can lead to side effects, drug interactions, and a higher likelihood of falls (NICE, 2023). Malnutrition, particularly in those living alone or in deprived areas, contributes to weight loss and frailty progression. Additionally, cognitive decline, including dementia and depression, exacerbates frailty and makes self-care increasingly difficult.
Mental Health and Social Isolation
Mental health plays a crucial role in overall well-being, yet conditions such as depression and anxiety often go unrecognised in older adults. Nearly 20% of older residents experience these conditions, which are frequently linked to bereavement, social isolation, and chronic illness (Age UK, 2022).
Dementia rates continue to rise, particularly in those aged 80 and over, placing increasing strain on both healthcare services and family caregivers. Social isolation is another pressing issue, particularly in rural areas, where limited transport and fewer community services contribute to loneliness and poorer health outcomes (Cumberland Council, 2023).
Social Determinants of Health
Older adults in Cumberland face several social determinants that significantly impact their health:
- Income and Poverty: Around 18% of elderly residents live in relative poverty, affecting their ability to afford nutritious food, home heating, and healthcare services (Joseph Rowntree Foundation, 2023).
- Housing Conditions: Older housing stock in rural areas often lacks age-friendly adaptations, making independent living more challenging.
- Transportation Barriers: Limited public transport options in rural areas restrict access to healthcare services, social activities, and essential amenities.
- Access to Healthcare: Rural health inequalities mean that older adults in remote areas face delays in receiving medical attention, leading to poorer health outcomes.
Potential Implications of These Trends
The decline in Healthy Life Expectancy in Cumberland raises significant concerns for healthy ageing policies. As more people spend a greater proportion of their later years in poor health, demand for healthcare, social care, and community support will rise. This challenge is particularly acute in rural areas where services are less accessible.
As Cumberland’s population continues to age, several key challenges are anticipated:
- Increased Demand for Services – Health and social care provision will need to expand, particularly for long-term care, palliative care, and chronic disease management. Greater service coverage will be required in rural areas to meet rising demand.
- Workforce Strain – The health and social care workforce will need to grow and adapt, ensuring there are sufficient trained professionals to support older adults with complex health needs (The King’s Fund, 2023).
- Economic Impact – A larger ageing population will place greater financial strain on public services, necessitating careful allocation of resources to address evolving priorities.
- Social Isolation Risks – Older adults, particularly in rural communities, are at heightened risk of loneliness and social exclusion due to limited transport, fewer local support networks, and restricted access to essential services (Age UK, 2022).
Addressing These Challenges Through Prevention
To reduce the impact of these trends, a stronger emphasis on preventative interventions is essential. Ensuring that older adults remain independent and maintain a good quality of life for longer will help relieve pressure on health and social care services.
Key areas for action include:
- Early diagnosis and better management of chronic conditions, helping older people to stay healthier for longer.
- Expanding access to physical and social activity programmes, promoting mobility, social engagement, and mental well-being.
- Reducing health inequalities through targeted local policies and investment in social care infrastructure, particularly in rural areas.
By prioritising prevention and early intervention, Cumberland can support healthy ageing, reduce pressure on care services, and create a more sustainable and equitable health system for future generations.