Cumberland is home to a wide range of services and initiatives aimed at promoting and improving the health and well-being of older adults. These services, provided by both statutory and third-sector organisations, play a crucial role in preventing social isolation, enhancing mobility, and ensuring access to essential healthcare and support systems. However, despite the breadth of services available, significant challenges remain. Rising demand, workforce shortages, and resource constraints are putting increasing pressure on service providers. Moreover, a small proportion of the population accounts for a large share of service provision, highlighting the need for a more radical and proactive approach to supporting older adults, particularly those managing frailty and multiple long-term conditions.
This chapter outlines the key services and initiatives in Cumberland that support older adults, with a particular focus on frailty management and healthy ageing. It also explores the challenges faced by these services and the innovative approaches being adopted to address them.
Community Support and Health Services
Cumberland offers a variety of community support and health services designed to help older adults live independently and maintain their health and well-being. These services are essential in reducing social isolation, enhancing physical health, and providing holistic healthcare support. Below are some key examples of these services:
Figure 10: Community support service for older adults
Frailty and Healthy Ageing
Frailty is often misunderstood. It is not simply an unavoidable part of getting older but a condition where the body gradually loses its ability to recover from illness, injury, or even everyday stresses. Some people remain active and independent well into their nineties, while others find themselves struggling much earlier. When frailty is poorly managed, even a minor infection or a small fall can result in significant loss of independence, hospitalisation, or long-term care.
However, frailty is not inevitable, nor does it have to mean a loss of quality of life. With the right preventative care, early identification, and tailored support, many older adults can continue to live well for longer. Cumberland is working towards a proactive, community-based approach to frailty that focuses on prevention, early intervention, and better integration between health and social care services.
The Growing Challenge of Frailty in Cumberland
As Cumberland’s population ages, frailty is becoming an increasingly urgent public health concern. National data shows that the prevalence of frailty is rising, reflecting broader demographic shifts in the UK. However, frailty is not just linked to ageing, it is heavily influenced by social and economic factors.
Recent local data from North Cumbria Integrated Care (NCIC) NHS Foundation Trust reinforces the scale of this challenge. Between 2022 and 2024, the number of hospital admissions for older adults (aged 65 and over) with frailty-related conditions increased by 33%, rising from 1,591 to 2,113 (Table 4). These figures reflect a growing burden on acute services and underscore the importance of preventative, community-based approaches to frailty.
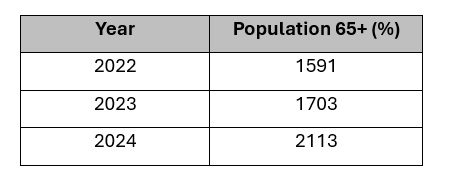
Table 4: Hospital Admissions for 65+ Patients with Frailty-Related ICD-10 Codes
Source: North Cumbria Integrated Care NHS Foundation Trust, 2025.
Alongside this, the proportion of older adults arriving in hospital with a Clinical Frailty Score (CFS) of 6 or more, indicating moderate to severe frailty, has been increasing over the past year. By January 2025, nearly one in three older patients (31.8%) fell into this category, up from 25.7% in March 2024 (Figure 11). This rising trend highlights the need for earlier identification and community-based support to reduce avoidable admissions and improve outcomes.
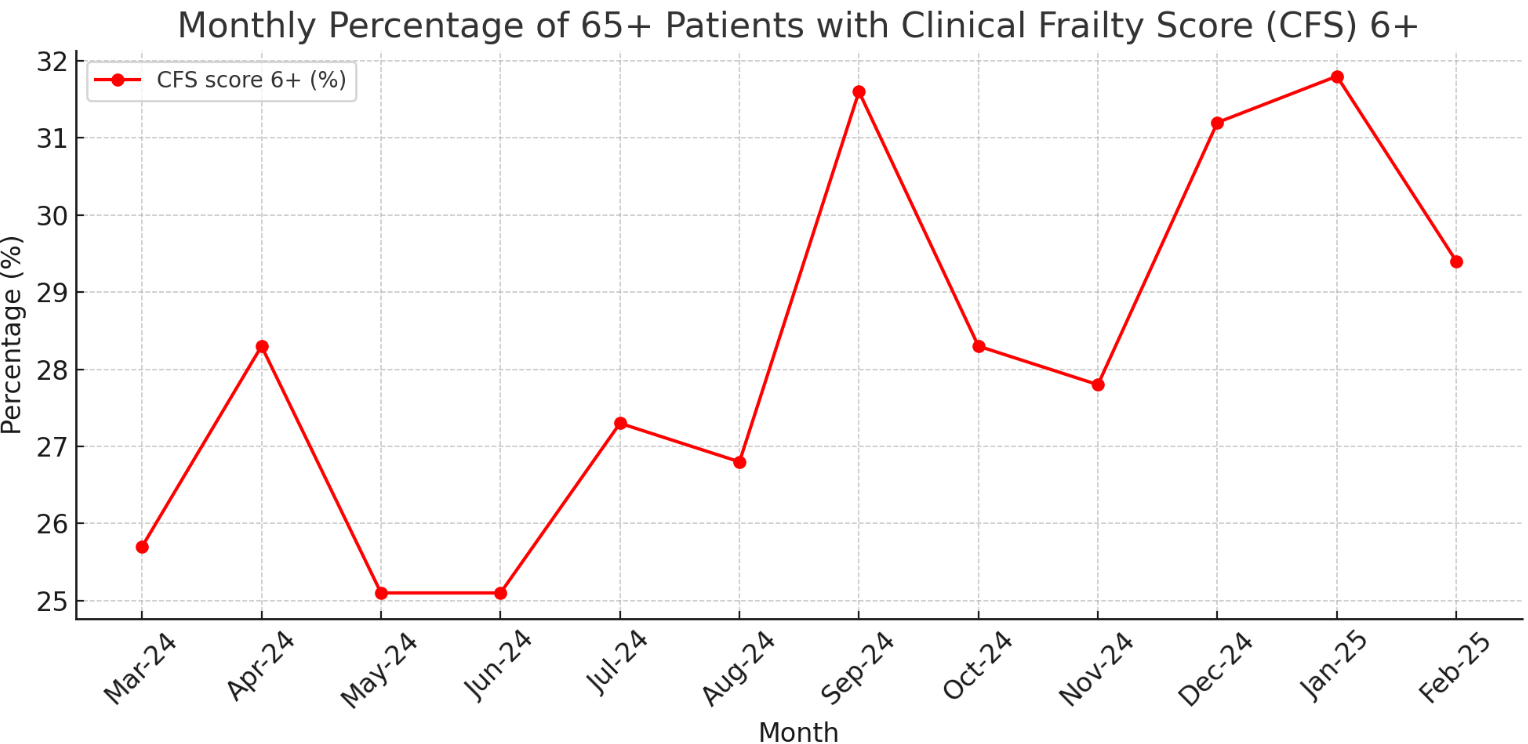
Figure 11: Monthly percentage of patients aged 65 and over with a Clinical Frailty Score (CFS) of 6 or above (March 2024 – February 2025)
Source: North Cumbria Integrated Care NHS Foundation Trust, 2025.
In addition, frailty score data collected over the past 104 weeks shows that fewer than 6% of older adults admitted to hospital were classified as ‘Very Fit’, while nearly half were recorded as mildly, moderately, or severely frail (Figure 12). These insights provide a valuable foundation for targeting interventions at those most at risk and for planning services around the needs of an ageing, increasingly frail population.
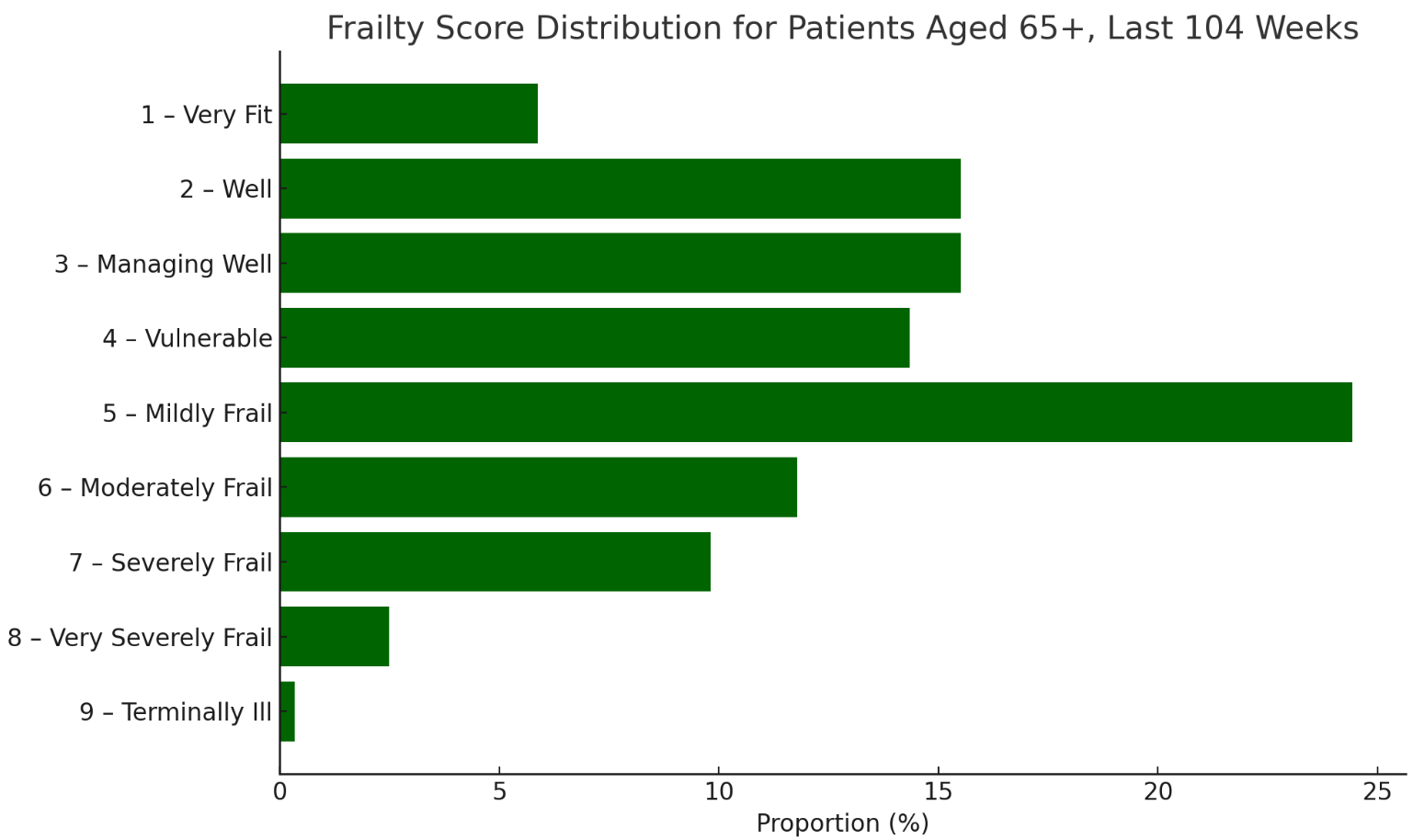
Figure 12: Frailty score distribution among patients aged 65 and over admitted to hospital, based on Clinical Frailty Scores recorded over the past 104 weeks
Source: North Cumbria Integrated Care NHS Foundation Trust, 2025.
Research indicates that individuals in deprived areas are twice as likely to experience frailty compared to those in more affluent communities (Sinclair et al., 2021). This pattern is reflected in Cumberland’s Primary Care Network (PCN) data, which highlights significant variations in frailty prevalence across different localities. People living in rural areas, those with long-term conditions, and individuals experiencing social isolation are at the greatest risk of developing frailty (Walsh et al., 2023).
Understanding these inequalities is essential in designing targeted interventions that address the needs of those most at risk. The approach taken in Cumberland is based on five key ambitions, aligning with the North Cumbria Frailty Strategy (2025-2029). These ambitions provide a structured framework for ensuring that older adults receive the right care, at the right time, in the right place (North Cumbria Place-Based Partnership, 2025).
1. Preventing Well: Staying Stronger for Longer
Frailty does not develop overnight, it is the result of gradual changes such as muscle loss, reduced mobility, poor nutrition, and social isolation. Without intervention, these small declines can lead to serious health deterioration. However, when caught early, frailty can be delayed, slowed, or even reversed.
Preventing frailty starts with keeping active, maintaining good nutrition, and raising awareness of early risk factors. Regular strength and balance exercises reduce falls and improve mobility (de Labra et al., 2015), while nutritional support and hydration programmes help combat frailty-related malnutrition (Lorenzo-López et al., 2017). Many people do not realise they are becoming frail until a crisis occurs, so increasing public and professional awareness is essential to encourage early action.
The Proactive Care Pilot Programme (2024) in North Cumbria represents a major shift towards prevention and early intervention. Traditionally, frailty has been managed reactively, with individuals only seeking help once they are already in crisis. This programme is designed to identify at-risk individuals sooner, ensure timely support, and strengthen community-led care (Year of Care Partnerships, 2024).
By shifting the focus to prevention rather than crisis management, Cumberland aims to reduce avoidable hospital admissions and improve long-term outcomes for older adults.
2. Diagnosing Well: Identifying Frailty Before It’s Too Late
Frailty often goes undiagnosed until a serious health event occurs. However, routine screening and early diagnosis can make a significant difference in preventing deterioration and ensuring people receive timely, personalised care.
To improve early detection, expansion of routine frailty screening in GP practices and community health settings Is crucial. Comprehensive Geriatric Assessments (CGA) are also being introduced to provide a structured, personalised approach to frailty management (Briggs et al., 2022). Alongside this, digital frailty indexes are being used to track trends and identify at-risk individuals before they experience a health crisis.
By embedding frailty assessment into primary care, Cumberland is taking a preventative, rather than reactive, approach to supporting older adults.
3. Supporting Well: Building a Care System That Works for Older Adults
For those already living with frailty, the right support can mean the difference between maintaining independence and frequent hospital stays. Cumberland is working to strengthen home-based care, expand carer support, and create a more joined-up health and social care system.
One of the biggest challenges in delivering frailty care is workforce shortages, particularly in rural areas, where high vacancy rates contribute to delays in accessing care (Cumberland Council, 2023). Cumberland is working to expand frailty-specialist roles, improve recruitment in rural areas, and develop mobile care models and telehealth services to bridge gaps.
Supporting people to stay at home safely is also a priority. Expanding assistive technology, home adaptations, and falls prevention programmes allows more people to live independently for longer. Carers play a vital role in frailty care, yet many struggle with little support. Increasing respite services, carer training, and access to financial advice is crucial in ensuring that carers are not left overwhelmed.
To reduce variation in care quality, Cumberland is developing a fully integrated frailty pathway, ensuring GPs, hospitals, social care teams, and community services work together. This approach will help reduce emergency admissions and ensure that older adults receive the right support, in the right place, at the right time.
4. Living Well: Supporting Independence and Wellbeing
Frailty care is not just about managing health conditions, it is also about supporting older adults to maintain purpose, independence, and connection to their communities. Social isolation and loneliness are significant contributors to frailty, affecting both physical and mental health. Ensuring that people remain socially engaged, financially secure, and able to access community services is just as important as medical care. A detailed discussion on social inclusion, loneliness, and community-based interventions can be found in the ‘Social Inclusion’ section of this report.
5. Dying Well: Ensuring Compassionate and Dignified Care
Similarly, planning for the later stages of frailty is essential. As people approach the end of life, having clear advance care plans, good palliative care, and family support ensures that they can receive care that aligns with their wishes. Many people express a desire to be cared for at home or in a familiar setting, yet a lack of early planning often leads to hospital admissions that could have been avoided. Cumberland is working to strengthen end-of-life care services and improve coordination between healthcare providers, social services, and families. These issues are explored further in the ‘Dying Well’ section of this report.
A Future Where Frailty is Managed
Cumberland is moving away from crisis-driven frailty care towards a system that prioritises prevention, early identification, and community-based support. By embedding the five ambitions for frailty into our local strategy, we can help older adults stay healthier, more independent, and better supported.
Frailty is a challenge, however through proactive, person-centred care, we can ensure that ageing in Cumberland is not just about living longer, but living well.