Ensuring individuals experience a dignified, comfortable, and well-supported end of life is a fundamental part of public health. In Cumberland, as in the rest of the UK, efforts continue to improve palliative and end-of-life care, supporting patients, families, and caregivers with high-quality, compassionate care that reflects personal preferences and needs. As the population ages, the demand for end-of-life services is increasing, necessitating a well-coordinated, multi-sector approach involving healthcare providers, social services, community organisations, and policymakers.
The North Cumbria End-of-Life Partnership (NCELP) plays a central role in shaping this approach, bringing together key stakeholders to develop a sustainable and equitable model of palliative care. This partnership ensures that Cumberland’s strategy aligns with regional priorities, with a focus on improving access, addressing health inequalities, and embedding best practice models for palliative care delivery (NCELP, 2024).
Current Landscape of End-Of-Life Care
Across the UK, many people express a preference to die at home or in a hospice, yet a significant proportion of deaths still occur in hospitals. In Cumberland, shifts in place of death trends over the past decade have been slow but noticeable.
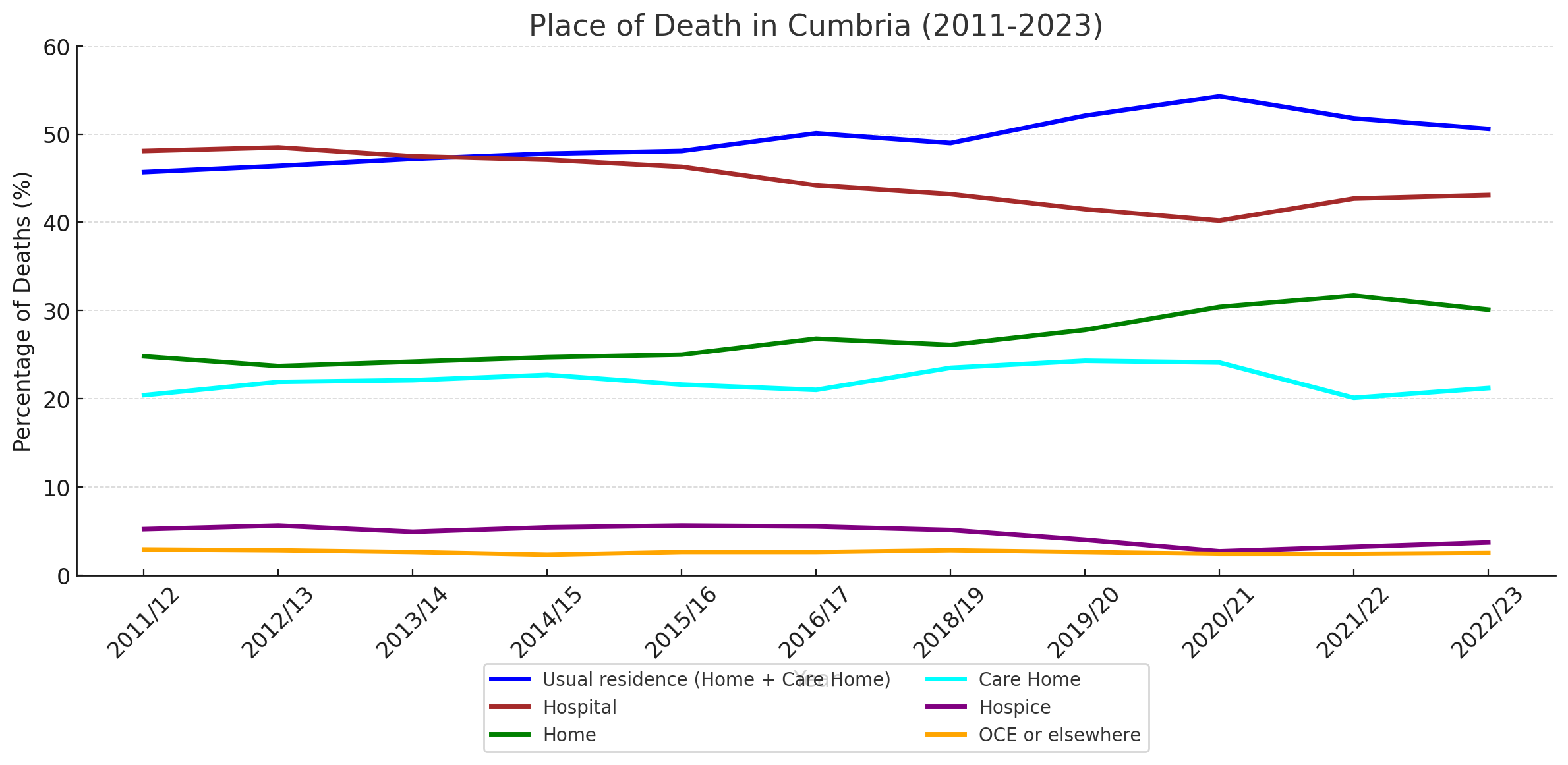
Figure 13: Summary of the Place of Death in Cumbria (2011–2023)
Source: Office for National Statistics (ONS), 2023
Figure 13 presents an overview of place of death in Cumberland from 2011 to 2023. Between 2011 and 2017, around 45% of people died in their usual residence (either at home or in a care home). By 2022/23, this had risen to just over 50%, indicating a steady increase in home-based and care home palliative care provision. Hospital deaths, while still accounting for a large proportion of deaths, have declined slightly, from nearly 50% in the early years to around 43% more recently.
Hospice deaths have remained low and stable throughout the period, consistently accounting for between 3% and 5% of total deaths. Deaths in ‘other’ settings, such as assisted living facilities or following emergency admissions, have also remained a small but consistent proportion of overall mortality.
Importantly, the combined data highlights the impact of the Covid-19 pandemic. In 2020/21, there was a marked increase in deaths occurring at home and in care homes, likely reflecting reduced hospital capacity and increased reliance on community-based care during the pandemic. While the data since then suggests a return to pre-pandemic trends, it is possible that some of the observed changes were driven by necessity rather than sustained improvements in service design or patient choice.
Overall, although it is encouraging that more people are dying in familiar settings, progress has been relatively slow. Hospitals continue to account for a significant proportion of deaths, and there remains substantial opportunity to further expand and strengthen community-based palliative and end-of-life care across Cumberland.
End-Of-Life Care Services in Cumberland
The North Cumbria Integrated Care NHS Foundation Trust (NCIC) provides a range of palliative care services for patients with life-limiting conditions. These services focus on:
- Managing pain and symptom relief.
- Providing emotional and psychological support for patients and families.
- Offering home-based palliative care to reduce unnecessary hospital admissions.
- Ensuring coordinated care planning between healthcare providers (NCIC, 2025).
NCELP has been instrumental in driving improvements in these services by fostering collaboration between primary care, hospices, and social care providers. However, delivering consistent, high-quality palliative care remains a challenge, particularly in rural areas where specialist teams may be harder to access.
Challenges in End-Of-Life Care
Disparities in Access to End-Of-Life Care
Older adults in rural Cumberland may experience limited access to specialist palliative care teams, hospice services, and community-based support, leading to an increased reliance on hospitals for end-of-life care. Ensuring that all residents have equitable access to palliative care remains a core focus of NCELP.
Workforce and Training Gaps
There is a shortage of trained palliative care professionals, including community nurses and end-of-life care coordinators. Expanding the palliative care workforce and training provision is essential to ensuring consistent, high-quality care (Kings Fund, 2023). NCELP is leading efforts to develop structured training programmes, ensuring that GPs, nurses, and social care workers are equipped to deliver compassionate, high-quality end-of-life care.
Delays in Care and Decision-Making
A lack of early discussions around advance care planning (ACP) means that some patients receive care that may not align with their preferences. Encouraging proactive ACP conversations between patients, families, and healthcare providers can help ensure greater autonomy and dignity in end-of-life decision-making.
Psychological and Emotional Support for Families
Providing bereavement support services is crucial in helping families and caregivers cope with loss and grief. Expanding specialist counselling and peer support programmes is vital to ensuring emotional well-being after the death of a loved one (NHS England, 2021).
Funding and Sustainability
One of the most pressing concerns is the financial sustainability of hospice and community-based palliative care services. Many hospices rely on charitable donations, short-term grants, and the Better Care Fund. However, without a stable funding model, these services remain vulnerable. NCELP is working with the ICB to develop long-term commissioning solutions that integrate palliative care into NHS funding streams, ensuring continuity of care for patients and families.
Policy Framework and Guidelines
End-of-life care in the UK is shaped by national frameworks and clinical guidelines that set best practices for high-quality, person-centred care.
- The National Institute for Health and Care Excellence (NICE) Guidelines NG31 outlines key principles for pain management, symptom control, and communication with families (NICE, 2015).
- Ambitions for Palliative and End-of-Life Care (2021-2026) provides a national framework for personalised, community-focused palliative care (NHS England, 2021).
- The NHS Long-Term Plan commits to expanding community-based palliative care services to allow more people to receive care in their preferred place of death (NHS England, 2022).
Cumberland is actively implementing these policies at a local level, ensuring that its palliative care services align with national ambitions for dignified, high-quality end-of-life care.
Local Initiatives in Cumberland
Expanding Community-Based Palliative Care
NCIC has been increasing palliative care services within community settings, aiming to reduce hospital deaths and ensure that patients receive holistic care closer to home (NCIC, 2025).
Hospice and Specialist End-of-Life Services
Local hospices, such as Eden Valley Hospice, continue to provide specialist palliative care, helping patients and families navigate end-of-life care with dignity (Eden Valley Hospice, 2024).
Advanced Care Planning Programmes
Efforts are being made to encourage earlier advance care planning, ensuring that patients can document their end-of-life preferences before a crisis occurs (Cumberland Council, 2024).
Bereavement and Family Support Services
Expanding grief counselling, emotional support groups, and practical bereavement guidance remains a priority, ensuring families receive the support they need (NHS England, 2021).
Advance Care Planning in Cumberland: Current Status and Opportunities for Development
Advance Care Planning (ACP) is a process that enables individuals to articulate their preferences for future medical care, ensuring that their wishes are respected even if they become unable to communicate them. Despite its importance, ACP remains under-used both nationally and within Cumberland.
Current State of Advance Care Planning in the UK
Despite the recognised importance of Advance Care Planning in ensuring that individuals' end-of-life care preferences are respected, engagement with ACP remains suboptimal across the UK. A 2013 survey by the British Medical Journal (BMJ) revealed that only 5% of British individuals had formalised an advance care plan, highlighting a significant gap in end-of-life preparedness (BMJ, 2013). Similarly, a 2017 report by Macmillan Cancer Support found that just 8% of people with cancer had discussed their end-of-life care preferences with a healthcare professional, further emphasising the lack of routine ACP discussions in clinical practice (Macmillan Cancer Support, 2017). The reluctance to engage in ACP conversations means that many end-of-life decisions are made reactively, often resulting in unwanted hospital admissions, aggressive treatments, and a reduced focus on palliative and comfort-centred care.
While ACP uptake remains low in the general population, care home residents show higher levels of engagement. A 2022 service evaluation found that 79.5% of UK care home residents had engaged in ACP, indicating that structured care environments may facilitate higher participation in advance care planning (Robinson et al., 2022). However, the study also highlighted significant inconsistencies in ACP implementation, with many care homes lacking the staffing, training, or resources to support ACP services effectively. Furthermore, gaps in communication between healthcare providers and care homes often lead to ACP preferences not being documented or honoured, undermining the intended benefits of these plans.
The data on Advance Care Planning engagement highlights a critical gap in end-of-life preparedness across the UK, with low national uptake and significant inconsistencies in implementation. The lack of routine ACP discussions means that many individuals do not have their care preferences documented, leading to reactive decision-making, increased hospital admissions, and potentially unwanted medical interventions. While ACP engagement is higher in care home settings, challenges such as staffing shortages, inadequate training, and poor communication between services limit its effectiveness.
For Cumberland, these findings reinforce the urgent need for structured ACP initiatives, including public awareness campaigns, professional training, and improved communication systems across healthcare providers. Additionally, there is a notable lack of comprehensive, up-to-date data on ACP coverage and adherence, making it difficult to assess how well ACP is integrated into healthcare systems and whether existing plans are being followed. Addressing this data gap will be crucial for developing evidence-based strategies that improve ACP uptake and ensure patients' end-of-life wishes are respected.
Barriers to Effective ACP Implementation
Several factors contribute to the underutilisation of ACP:
- Cultural and Emotional Challenges: Discussing end-of-life care is often considered taboo, leading to discomfort among patients and healthcare professionals. This discomfort can result in the avoidance of crucial conversations about future healthcare preferences (BMC Palliative Care, 2020).
- Lack of Education and Training: Healthcare professionals frequently report insufficient training in initiating ACP discussions. A study highlighted that the primary barriers to ACP include a lack of understanding and knowledge, as well as discomfort and resistance among healthcare providers (Journal of Hospice and Palliative Care, 2023).
- Time Constraints: The demanding nature of healthcare settings often leaves limited time for in-depth ACP discussions. This time pressure can prevent healthcare providers from engaging in meaningful conversations with patients about their end-of-life preferences (PubMed, 2019).
- Communication Gaps Among Services: Even when ACPs are in place, there is often a lack of effective communication between various healthcare providers, including general practitioners, community nurses, healthcare assistants, and emergency services. This disconnect can lead to situations where ACPs are not honoured due to unawareness among care teams.
Strategies for Enhancing ACP Engagement
Engagement with ACPs remains inconsistent, with many delaying discussions until a crisis arises. The North Cumbria End-of-Life Partnership (NCELP, 2024) highlights ACP as a priority, calling for a structured, proactive approach across Cumberland.
1. Public Education and Awareness
Raising awareness is crucial to normalising ACP discussions. Many people are unaware of its benefits or feel uncomfortable initiating conversations. The NCELP strategy highlights the need for targeted public education through community outreach, accessible materials, and engagement with underserved populations. Presenting ACP as a routine part of healthcare will encourage earlier decision-making.
2. Workforce Training
Healthcare professionals often lack confidence in discussing ACP. The NCELP strategy calls for structured training for GPs, nurses, and palliative care teams, ensuring they can guide patients sensitively and effectively. ACP education should be embedded into routine professional development, equipping all frontline staff with the necessary skills.
3. Embedding ACP into Healthcare Pathways
ACP must be integrated into routine care rather than treated as an isolated task. The NCELP strategy recommends incorporating ACP into long-term condition management, particularly for those with chronic illnesses or frailty. Using structured tools within primary care records will ensure ACP discussions are documented, updated, and revisited when necessary.
4. Improving Communication and Information Sharing
A major barrier to ACP is poor communication between services. The NCELP strategy highlights the need for shared digital records so that ACP decisions are accessible across GPs, hospitals, hospices, and care homes. Standardised protocols will ensure healthcare teams follow a consistent approach, reducing the risk of preferences being overlooked.
5. Strengthening Policy and Leadership
Embedding ACP into local commissioning plans is essential for long-term sustainability. The NCELP strategy calls for support from the ICB to prioritise ACP, secure funding for training and public awareness, and monitor uptake to address gaps. A coordinated approach will improve consistency across Cumberland’s health and care system.
By addressing these barriers and implementing targeted strategies, Cumberland can enhance the adoption and effectiveness of Advance Care Planning, ensuring that individuals' end-of-life preferences are respected and upheld.
Future Directions
End-of-life care in Cumberland needs to continue evolving towards a more community-based, person-centred approach, ensuring people can receive care where they feel most comfortable. Expanding hospice-at-home services and strengthening community palliative care will help reduce unnecessary hospital admissions and improve quality of life in the final stages. The North Cumbria End-of-Life Partnership (NCELP, 2024) is leading efforts to make this happen by focusing on workforce development, better coordination between services, and digital record-sharing to ensure seamless care.
A skilled and confident workforce is key to delivering high-quality palliative care. While there is a need for more specialist nurses and palliative care consultants, the NCELP strategy also highlights the importance of training GPs, community nurses, and social care workers, so they feel equipped to provide compassionate, end-of-life care. Advance Care Planning should become a routine part of healthcare, rather than something left until a crisis. Ensuring ACP discussions happen earlier, and that preferences are properly recorded and easily shared across healthcare services, will give people greater control over their final months.
Bereavement support also needs to be better integrated into palliative care, ensuring families and carers receive the emotional and practical help they need. Achieving all of this will require ongoing collaboration across health, social care, and voluntary sectors. By improving training, communication, and access to community-based care, Cumberland can help more people experience a dignified and well-supported end of life, in line with their wishes.